 Since the release of the Advanced Notice of Proposed Rulemaking (ANPRM) approximately 1 year ago, the talk in SNF Rehab Departments has been about RCS-1 and the looming potential changes coming down the road that would not only change reimbursement for Medicare Part A , but impact the way therapy is currently provided. Along with the facts about RCS-1, there were many many myths and rumors as to how therapy life in the SNF would forever change. See our last article “RCS-1: To be or not to be.
Since the release of the Advanced Notice of Proposed Rulemaking (ANPRM) approximately 1 year ago, the talk in SNF Rehab Departments has been about RCS-1 and the looming potential changes coming down the road that would not only change reimbursement for Medicare Part A , but impact the way therapy is currently provided. Along with the facts about RCS-1, there were many many myths and rumors as to how therapy life in the SNF would forever change. See our last article “RCS-1: To be or not to be.
Therapists nationwide were awaiting the SNF PPS Proposed Rule due to be released this spring, in hopes of getting clarification on the changes to come. {For those new to the process, the Proposed Rule released each year outlines changes for the start of the next FY (Fiscal Year) which starts on October 1st. It is released to allow time for comments from providers before releasing the Final Rule prior to October 1st.}
We knew changes were coming, however, as of last month in an ODF (Open Door Forum), CMS stated they were still analyzing comments and feedback related to the proposed changes…and official policies and a start date had not yet been set.
…and then yesterday, April 27th, CMS released the anticipated 266 page Proposed Rule. Yes, change is coming…but not until October 1, 2019….and it was NOT RCS-1!
This new rule proposes the replacement of the existing case-mix classification methodology, the Resource Utilization Groups, Version IV (RUG-IV) model, with a revised case-mix methodology called the Patient-Driven Payment Model (PDPM) effective October 1, 2019. RCS-1 was essentially revamped in response to comments and additional data analysis….and then renamed.
So What Happened?
Well, CMS has commented in the Final Rule for at least the last 5 years that there was significant concern regarding the therapy trends in the SNF . CMS has cited 2 concerns in particular:
- The percentage of residents classifying into the Ultra-High therapy category has increased steadily (reaching >60% of total scores in 2017)
- The percentage of residents receiving just enough therapy to surpass the Ultra-High and Very-High therapy thresholds has also increased (some SNF’s achieved 100% of RU and RV RUGS with exact minutes of 720 and 500 respectively…like magic)
In the 2015 SNF PPS Final Rule, CMS stated: “We believe the increase in “thresholding” is a strong indication of service provision predicated on financial considerations rather than resident need.” “….Therefore, services which are not specifically tailored to meet the individualized needs and goals of the resident, based on the resident’s condition and the evaluation and judgment of the resident’s clinicians, may not meet [the] definition for covered SNF care, and we believe that internal provider rules should not seek to circumvent the Medicare statute, regulations and policies, or the professional judgment of clinicians.”
{Did you know CMS said this? Looks like they may have been on “your side” all along….though not all were listening….}
So, after years of recommendations and clear data from the OIG and MedPAC to make a change, CMS took a stand last May, gave fair warning of a new payment system (RCS-1) and allowed comments for an extended period of time. CMS really did listen to all the comments and concerns about RCS-1, took them into account and created a payment model with a new name – PDPM.
For those not paying attention to the multitude of CMS statements over the years reiterating that therapy service provision should be based on the resident’s individual needs, this Proposed Rule would rename the payment model so no one could forget… The Rule states:
To make clear the purpose and intent of replacing the existing RUG-IV system, the model we are proposing in this rule is called the Patient-Driven Payment Model (PDPM).
Ok, got it! Patient-Driven…..not therapy-driven, not minute-driven!
Nuts and Bolts of the new PDPM?
PDPM is a new payment model, very similar to the previously proposed RCS-1, that sets daily Medicare Part A payment rates on factors other than therapy days and minutes. Data from the MDS, starting with the ICD-10 code and category that supports the SNF Part A stay, are used to classify a resident. Additional MDS data including function, cognition, swallowing disorders and other clinical diagnoses also contribute to classifications. Unlike the RUG-IV classification where each resident is only classified into 1 RUG group based on the MDS, PDPM breaks apart therapy and nursing to allow for a separate classification for each.
Here is a breakdown of the contributing components:
Nursing is finally “free” from therapy’s grip. With RUG-IV, Rehab RUG’s often trumped Nursing RUG’s. PDPM will use a similar set up as RUG-IV for nursing, minus the Rehab RUG’s. RCS-1 had the total # of RUGS down from 66 to 43, and now PDPM takes it down even further to a total of 25 by combining existing groups. The method for calculating the ADL score will also change and Section GG items will be added to the mix.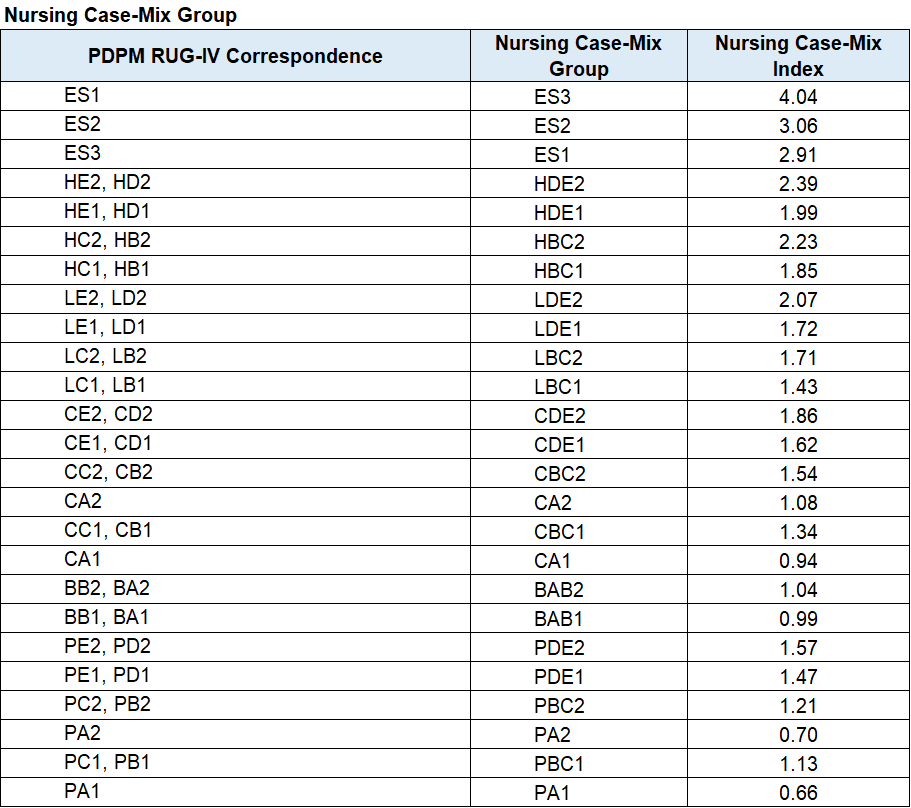
PT case mix and payment will be determined by the ICD-10 code category for SNF admission and the functional score based on MDS questions. There are a total of 16 potential PT case mix groups as show here,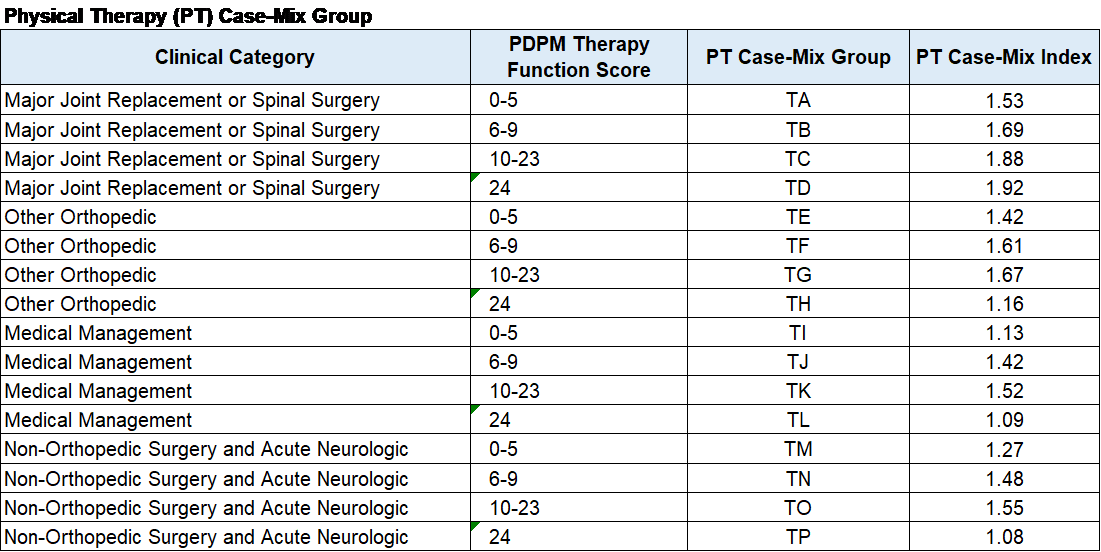
OT case mix and payment are determined exactly like PT, however, case mix scores and payment will differ for each category. 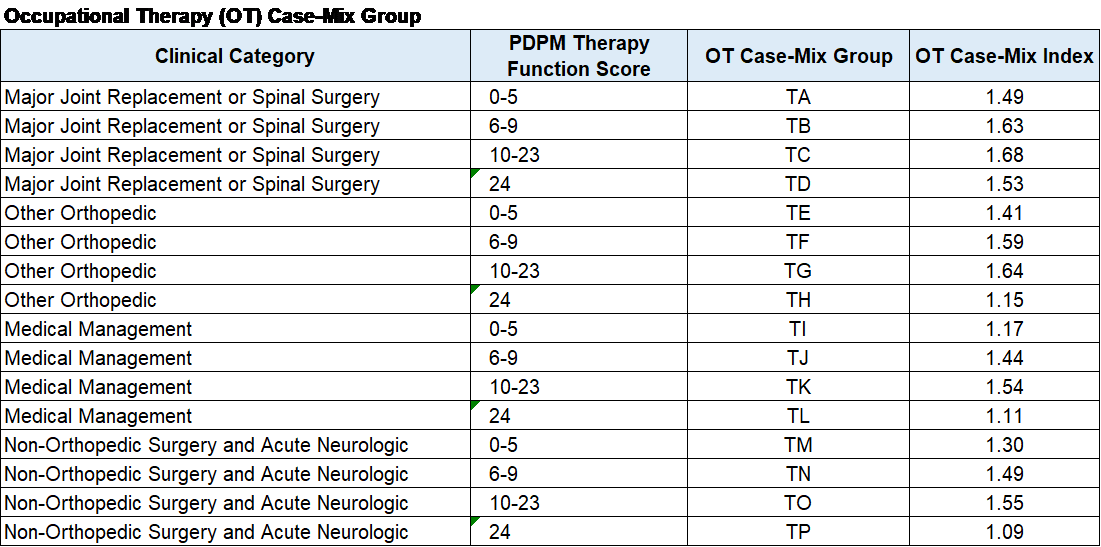
Of note, the daily payment amount for PT and OT will pay the full rate for the first 20 days and then decrease by 2% every 7 days thereafter for the remaining 80 days.
Speech case mix and payment is determined by the ICD-10 code category for SNF admission, as well as factors including swallowing disorders, mechanically altered diets, speech co-morbidities and cognition (all from MDS answers). The daily speech rate does not decrease over time like the PT and OT rates.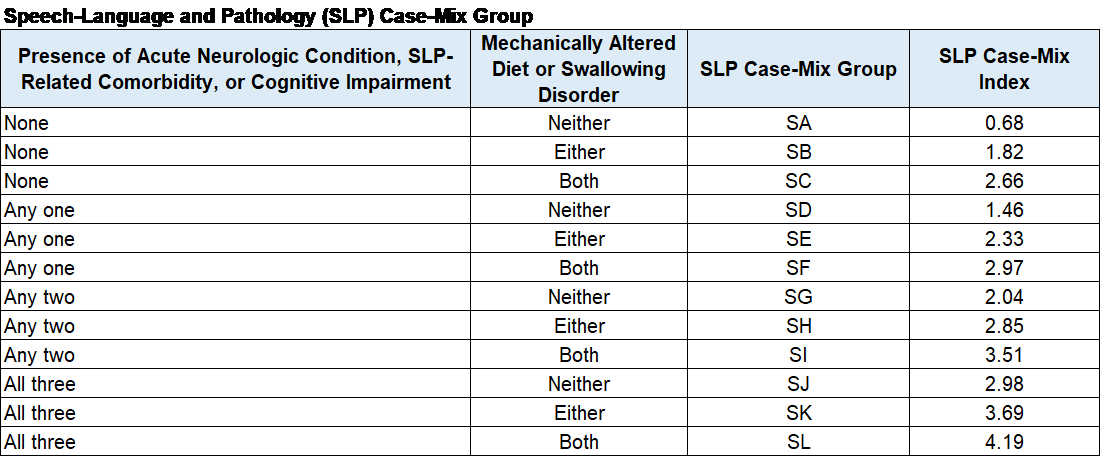
Now remember….minutes don’t matter. In fact, these PT, OT and Speech categories/case-mix are not even impacted by the presence or absence of an active therapy program. Each resident will fall into a PT, OT and SLP case mix group regardless of therapy services. Yes….facilities are paid a daily rate for therapy services even if therapy is not active. If therapy is active, the payment rate does not change with the amount of time spent with the resident. Why? CMS expects the SNF to save payment for when therapy services are necessary.
There is also a case mix category called “Non-Therapy Ancillary” that will use MDS questions from Section I, K, M and O to determine a case mix score. This payment is tripled for the first 3 days of the stay to cover any costs upfront.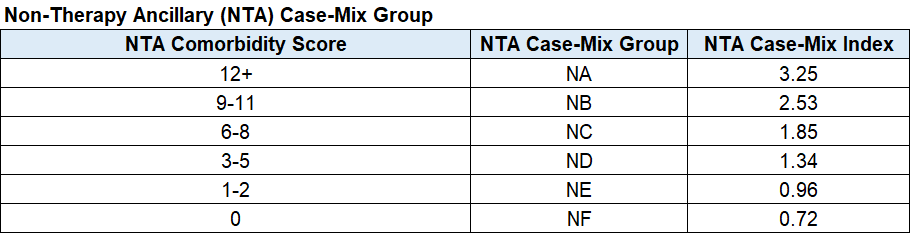
In addition to the 5 case mix based categories above, there is also a non-case mix payment (flat rate) for “overhead costs” such as room and board, laundry, capital expenses, dietary, etc.
The payment rate for the above 6 categories will be added up to make the total daily per diem payment rate. So with RUG-IV we had 1 category determining daily payment and now with PDPM, the eggs are spread into 6 baskets.
What Can Therapists Do To Prepare?
Read the Proposed Rule! It is only 266 pages. You may not need all the info in there, but it will give you greater perspective on why changes were made and the data that drove the changes. It also gives you insight into Medicare’s thought process for Part A payment.
Education is always the best bet. If you are not familiar with the MDS, now is the time to get your feet wet. The MDS tool is and will continue to be the central point for outcomes, Part A reimbursement, Quality Measures, Star Ratings, State case mix and more.
Oh, and there is so much more info out there if you are interested. Here are a few links to get you started.
SNF PPS Proposed Rule for Oct 1st 2018
Acumen Technical Report – SNF PPS Data for PDPM – April 2018
SNF PPS Payment Driven Payment Model CMS Webpage
*Keep in mind that this is a Proposed Rule…and things may change as the date approaches.
Will SNF Therapy Change When “Minutes Won’t Matter?”
Technically it shouldn’t. But will they? Possibly initially…until the dust settles.
If your facility was providing therapy services based on resident’s need and not financial targets, nothing should change, right? CMS used existing provider data to revamp the payment system, and says that if your facility was not one that provided an “excess” of Rehab Ultra, you may be looking at a significant increase in reimbursement under the new model. However, if your facility was one of those with a super high percentage of Ultra High RUG’s, your facility may see a dip in reimbursement with PDPM.
CMS put out a comparison tool so facilities could look themselves up to see how reimbursement would change under PDPM assuming all other variables stayed the same. Find your facility (you will need to know your CCN number) and see what the difference (+ or -) would be if PDPM was in effect in 2017. You can also see your facility revenue which may be eye opening for you!
PDPM Comparison Tool (It is an excel file that you can download and search for your facility. Compare revenue under RUG-IV with PDPM.)
So….
Don’t fall into the doomsday mode out there! There is plenty of Medicare Part A dollars that will continue to be available in the system. You just need to find a facility or company that is willing to “share” with you! Now is the time to find a facility or company that sees you for your value BEYOND your ability to provide minutes!
A new payment model may be a blessing in disguise for therapists in the SNF setting. Therapists who have been around since pre-PPS {cough} remember what autonomy felt like and remember not only being able to make a difference in each residents life, but the life of the SNF as a whole. Back then, therapists were team players that knew the rules…knew what the DOH was looking for…knew what the big picture looked like . Therapists have always been team players, but let’s be honest here…therapist autonomy was somewhat hijacked when PPS and managed Rehab departments came into play.
If you have questions about PDPM or anything else SNF related, send them to our Just Ask Q&A Forum and our team will help you out.
In Your Corner,
Dolores and the Montero Therapy Team

Are there any new regulations relating to PT billing with wound debridement?
Hi Kim – Any changes in this area would have been in the Physician Fee Schedule Final Rule last year with changes taking effect 1/1/19. I don’t recall any specific CPT code changes for CY2019 in this area. Hope that helps!