Welcome to Part 4 of our “Finding Your Balance” Blog Series
Just in case you missed Part 1, 2 or 3, here are the links:
Our goal with this Blog Series is to provide the therapist working in long-term care {and geriatrics} with a series of clinically relevant objective tests and measures that can be used in your department. For each of the tests reviewed here, we will give you:
- The “how to”
- The “pros and cons”
- The statistical measures
- The “norms” for the geriatric population
- A ready-to-use printout of a customized test form that you can use in your setting immediately
This objective data should be included in your clinical documentation and will support the necessity of your services and help support your goals and treatment plan. Not only that, but you will gain valuable insight into the specific limitations of your residents and be able to develop a natural progressive treatment plan to keep them on their feet! If you use an EMR, no worries, you can reference the test score in your electronic documentation and keep the paper copy in your soft chart. Remember, Medicare is looking for objective clinical data– so why not give it to them!!
A Quick Recap: Measuring Balance
When selecting a test to measure balance, there are multiple factors therapists consider, which ultimately help match up a test to our resident.
- How practical is the test?
- Is the test easy to administer?
- Can the test be incorporated into a treatment session?
- Is it cost effective?
- Is equipment required?
- Statistically is it a “good” test — is it reliable, valid, reproducible?
For our geriatric residents, there are also multiple additional considerations including: cognition, medications and interactions, sensory impairments, endurance and the severity of the balance impairment we are attempting to measure… just to name a few.
The Four Square Step Test (FSST)
What Does It Measure: Measures dynamic standing balance and identifies fall risk. Developed to assess the rapid change in direction while stepping forward, back and sideways over a low obstacle. Assesses dynamic balance, stepping, weight shift, spacial ability and sequencing skills.
How Long Does It Take: < 5 minutes
Equipment Needed: 4 straight canes (or dowel-type objects of 2.5 cm height that can remain stationary); stopwatch; 10 square feet of space;
How To: Step-by-step test instructions below. A clinic-ready documentation template can be printed out for clinic use by clicking the download button below.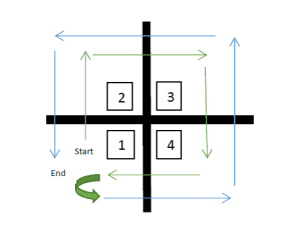
- Place 4 canes in a + pattern on the floor. Secure them so they don’t roll.
- Label the lower left square 1, and move clockwise to label 2, 3 and 4.
- Have your patient stand in square 1, facing square 2. Facilitate the movement pattern in the picture: Step forward to 2, step right to 3, step back to 4 and step left to 1. Then reverse the sequence: step right to 4, step forward to 3, step left to 2 and step back to 1.
- Both feet must touch in each square. Instruct patient “Try to complete the sequence as fast as possible wihtout touching the sticks. If possible face forward during the entire sequence.”
- Demonstrate the sequence for the patient. Then allow one practice trial.
- Complete 2 tests and use the best time as the score.
- Start time when first foot contacts floor in square 2, end time when last foot contacts floor in square 1.
- Provide close supervision throughout due to risk of tripping.
- A cane is allowed as an assistive device for the test.
- If patient hits a cane with foot or has loss of balance, no score is given and the trial is repeated.
Norms:
Normative values varied widely based on population studied. In general, norms are as follows:
<15 Seconds: Not at risk for falls
>15 Seconds: At risk for multiple falls
Inability to complete test without contacting canes: Significant fall risk
Results:
Valid (correlates at p<.001) with other tests proven to be valid (ie: TUG); Reliable; Reproducible; Positive predictive value of 86% and negative predictive value of 94% at 15 seconds (Dite and Temple 2002)
Pros:
Valid and reliable measure of balance; Excellent prediction of fall risk; Little space and equipment needed; Incorporates rapid, complete weight shifting while changing direction, as well as stepping over low objects.
Cons:
Requires cognitive level to remember and carry out sequence; Requires skilled supervision by tester to prevent falls; No score if not able to complete test.
Print Out of Test and Documentation Form From the Toolbox
Documentation, Billing and Treatment Ideas
The initial performance of the test can be incorporated into an initial evaluation or performed separately at any time during the course of treatment. If the test is performed on the initial evaluation, the score can be documented and used to establish short and long term goals for balance improvement, or “fall risk reduction.” Subsequent repeat performances of the test can be done during a treatment session and the time can be allocated to CPT 97112, neuro muscular re-education, a time-based code incorporating therapeutic procedures to improve balance, coordination, kinesthetic sense, posture, and proprioception. If you choose to use balance as a measure for your Functional Limitation Reporting, the G-Code Category “Changing and Maintaining Body Position” is appropriate, with G8981 for the Current Status, G8982 for the Goal Status and G8983 for the Discharge Status.
Treatment sessions can include portions of the test incorporated into treatment activities by marking a + on the treatment area floor with tape. Canes can be added to the + once patient has progressed to this level. Cognitive, problem solving, strength and sequencing tasks can be incorporated into the activities based on patient needs. For example:
- Practice stepping in different directions on therapist command (1, 3, 2, 1, 4….)
- Practice following commands and coordination: “Place left foot in square 2.”
- Stepping in all planes with weights on ankles
- Stepping with eyes open/closed
- Stepping while holding object in hand/hands
- Use colors, symbols or letters on the floor instead of numbers for cognitive tasks
- Use the lines of the + for balance beams
- Be creative!
In Summary
Our patients/residents like to see evidence that they are progressing, as well as challenges, tests and comparison with their peers. The Four Square Step Test allows them to see that they are performing tasks with less loss of balance, and that provides positive reinforcement to continue to progress toward goals. This is an easy test to perform in therapy sessions and therapy treatments can be derived from a set-up of the four squares. Why not familiarize yourself with it today!
Whether you are screening residents for fall risk or providing treatment to residents with balance deficits, if you have not been using objective tests and measures for balance, the FSST is a great place to start. Try it with your higher level balance patients today!
Have some fun and test yourself first!
Any questions, Just Ask! by visiting our Q&A forum.
In Your Corner,
Dolores
*A special thank you to physical therapist extraordinaire, Laura Minnick, for contributions to this post.
Dolores Montero, PT, DPT, GCS, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team @ MonteroTherapyServices.com
