Change is no longer a “shocker” in the therapy world.  So the news of more upcoming changes should be taken in stride by physical and occupational therapists…in particular, those using CPT® Codes (Current Procedural Terminology) as part of their daily coding and billing practice.
So the news of more upcoming changes should be taken in stride by physical and occupational therapists…in particular, those using CPT® Codes (Current Procedural Terminology) as part of their daily coding and billing practice.
PT’s and OT’s have used the “Evaluation Codes” 97001 – PT Evaluation and 97003 – OT Evaluation for years upon years. Well….say goodbye at of the start of 2017. These Evaluation Codes, along with the 2 “Re-evaluation Codes,” 97002-PT Re-evaluation and 97004-OT Re-evaluation, will be forever deleted and replaced with 8 new codes!
So much for simplicity!
How Did This Happen?
Every year, Center for Medicare and Medicaid Services (CMS) publishes the new Medicare Physician Fee Schedule (PFS) that, in part, sets the payment rates and rules for Medicare Part B in the SNF setting {and all other settings providing Part B “outpatient” therapy services.} The Proposed Rule that was presented in July contained updates in payment policy and payment rates that would go into effect on January 1st, 2017 if not changed in the Final Rule. You can find the Proposed Rule here: CY 2017 Medicare Physician Fee Schedule Proposed Rule
The Proposed Rule addressed the PT and OT Evaluation and Re-evaluation codes {as well as other therapy issues that we will discuss in a separate article.} The Final Rule won’t be out until October or November, but here is what we can expect.
The {old} evaluation codes will be deleted. Say goodbye to:
- 97001: PT Evaluation
- 97002: PT Re-evaluation
- 97003: OT Evaluation
- 97004: OT Re-evaluation
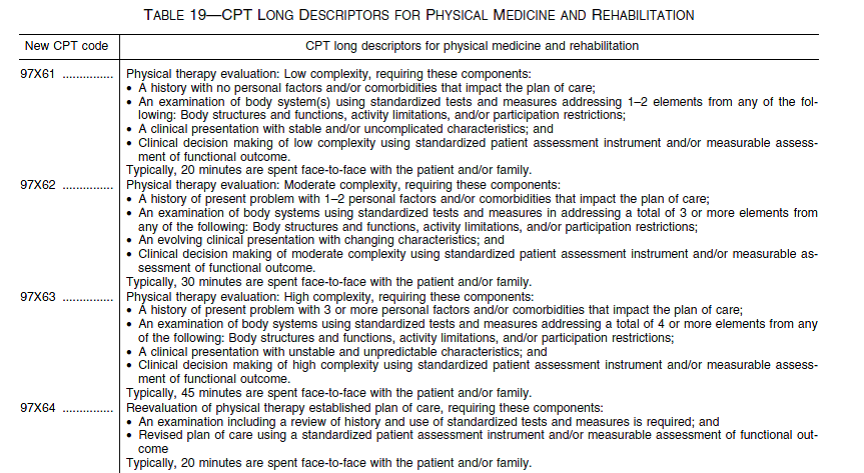
The codes will be replaced with a set of tiered codes based on level of complexity. The complexity of the evaluation will be coded based on low, moderate or high levels. Say hello to:
- 97×61: PT Evaluation – Low complexity
- 97×62: PT Evaluation – Moderate complexity
- 97×63: PT Evaluation – High complexity
- 97×64: PT Re-evaluation
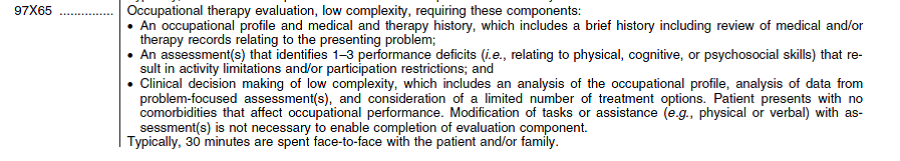
- 97×65: OT Evaluation – Low complexity
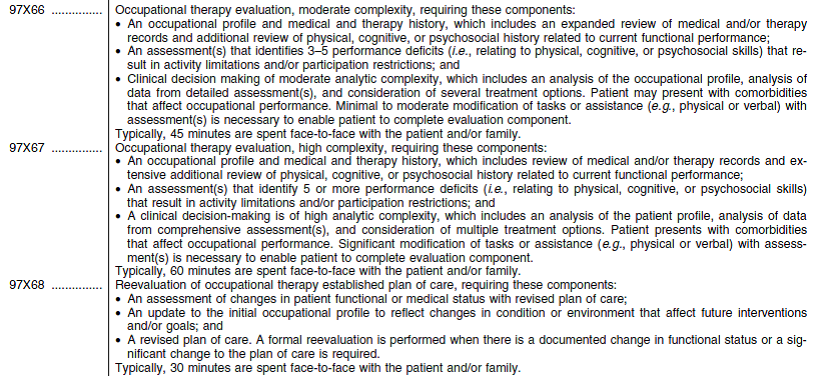
- 97×66: OT Evaluation – Moderate complexity
- 97×67: OT Evaluation – High complexity
- 97×68: OT Re-evaluation
Each code has a defined use and must meet specific criteria for use based on face-to face time spent, standardized tests used, comorbidities and performance deficits identified. More on all that later…For now, take a look at the codes and descriptors below.
The New PT Evaluation and Re-Evaluation Codes and Descriptors
The New OT Evaluation and Re-Evaluation Codes and Descriptors
How Will Payment Change?
For now, all levels will pay the same rate vs assigning different payment/reimbursement rates to each code based on complexity. This was not the AMA, APTA and AOTA recommendation and APTA has expressed “deep disappointment” with this decision to keep payment the same for all levels since each level is significantly different. You can read APTA’s statement here.
The CPT Editorial Panel’s creation of the new codes for PT and OT evaluative procedures grew out of a CPT workgroup that was originally convened in January 2012 when contemplating major revision of the Physical Medicine and Rehabilitation CPT section of codes. With the implementation of the new tiered codes, the intention was to also adjust the RVU (Relative Value Units), though CMS did not bite. The RVU is part of the formula Medicare uses to calculate payments for the services you provide for each CPT code, and adjusting the RVU for each, would adjust payment. If CMS does not include the stratified payment values in the Final Rule {coming out this Oct/Nov}, APTA strongly urged the agency to delay any future payment adjustments that would be based on analysis of claims filed in 2017 under the new codes.
What’s Next?
First, we wait to see what the Final Rule says in October, though we will likely not see a change from the above. Second, we educate ourselves as to the new codes and definitions now so that we will be ready to code accurately and responsibly in January. Keep in mind that even if all codes will “pay the same” in 2017, this will not be the case moving forward. CMS has indicated that they will analyze how therapists use the codes and levels in 2017 and then make determinations on their value based on the data they collect. The patterns that we establish now will impact us later! So Code Choices matter!
Your EMR software will update with the new codes and if you are still on paper you will need to make room for the 8 new codes, or a total of 6 extra codes. Your documentation process should also be reviewed. Are you documenting about co-morbidities? Are you using standardized tests? Are you documenting on all of the “performance deficits” found on evaluation? How many minutes are you currently documenting for your evaluation?
Keep an eye out for updates. Keep yourself in the loop and ahead of the curve!
In Your Corner,
Dolores
For those of you in New York and the surrounding areas, join us on October 1st to review these and all other upcoming changes impacting the SNF therapy world. Click here for conference details.
