CMS released the Physician Fee Schedule (PFS) Final Rule, a.k.a. the “Medicare Part B Rule,” outlining changes that will go into effect on 1/1/26.
This 1,200+ page document includes information for all Part B settings on payment rate changes, codes changes, telehealth and more. We pulled out the Medicare Part B rules that impact therapy in the SNF setting.
Final Changes For January 1st, 2026
1. Rate Information
Rate cuts for Part B have been the norm in recent years. Last year, the decrease in average payment rate under the Physician Fee Schedule (PFS) was 2.9%. This year, we have “good news and bad news”…..
- Good News: CMS proposed a 3.26% increase
- Bad News: SNF Therapy providers may not see the full increase
Each year, determining the rate for individual Current Procedural Terminology (CPT) Codes is a balance of variables, including the Conversion Factor (CF), which typically changes annually, and Relative Value Units (RVU) for each CPT Code, which are less likely to change. While each CPT Code has its own RVU, the CF is applied equally across all Codes, meaning, if the CF is the only variable changing, then the outcome for each CPT Code rate will be determined by an increase or decrease in the CF. If the CF stays constant, the outcome will be determined by any change in the RVUs. You get the idea…
The CF has been trending down for almost a decade, dragging the value of many CPT Codes with it. For CY2026, however, CMS is finalizing a 3.26% increase in the CF, from $32.35 last year, to $33.40 this year.
- 3.3% = [0.25% Fee Schedule Increase + 2.5% from the Big Beautiful Bill, and a 0.49% neutrality adjustment]
However, SNF therapy providers may not see that full increase due to reductions in the “other variable,” Relative Value Units (RVU), that CMS is adjusting for many CPT Codes.
CMS finalized a decrease in RVUs for many of the CPT Codes for CY2026, counteracting the increases gained from a higher CF for all CPT codes. The result… CPT Codes with no change in their RVU will see that 3.26% increase. CPT codes with a reduction in the RVU will see less than 3.3% increase, all depending on the RVU of each Code.
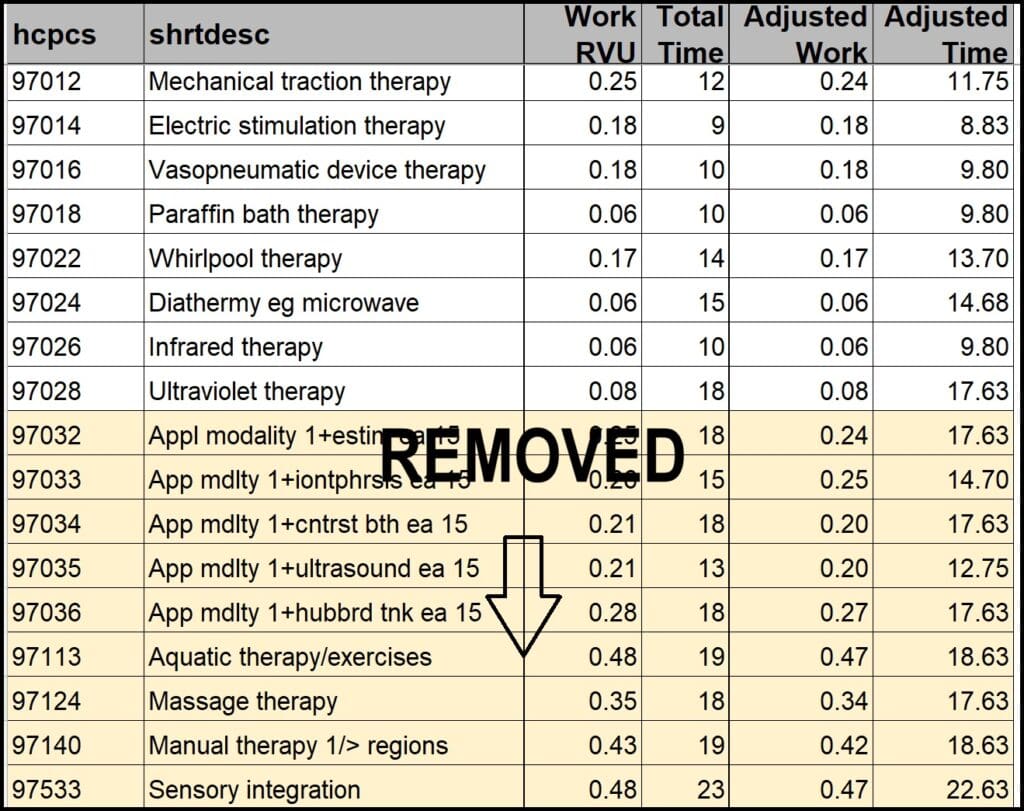
The Final Rule targets non-time-based CPT codes for the RVU reduction through an “efficiency adjustment” of -2.5%. CMS states the reduction is due to clinicians being “more efficient” in providing these services and is equating this to requiring less reimbursement. So much for being good at your job!
“We are finalizing this efficiency adjustment to all codes except time-based codes, including but not limited to, E/M visits, care management services, behavioral health services, services on the CMS telehealth list….”
In the Final Rule, CMS corrected the issue of including some of the therapy time-based codes in the mix (highlighted below) in the Proposed Rule. This snapshot lists the therapy non-time based codes that will see the efficiency adjustment, as well as the removal of the time-based codes that were included in error.
Because each CPT Code has its own RVU, each provider will be impacted differently. Providers that frequently bill the impacted codes will see a bigger hit than those that don’t.
The silver lining here for SNF therapy is that the true non-time-based codes listed here are not frequently used in most SNF Part B settings.
Here is the link to the CMS file of impacted CPT codes:
CY 2026 PFS Final Rule Codes Subject to Efficiency Adjustment – Updated 11/17/2025
Did you know you can look up any CPT code and check the reimbursement rate HERE ?
If you haven’t done so yet, download our custom CPT Code tool with all PT, OT and SLP codes, code definitions and code category (time-based/pays by unit vs non-time-based/pays flat rate) to help keep track of the information.
Download SNF Therapy CPT Cheat Sheet
2. Modifiers + Manual Medical Reviews
KX Modifier Threshold
The “old” Therapy Cap is now disguised as the KX Modifier Threshold, and “threshold amounts” change yearly. The 2025 “threshold” of $2,410 for OT, $2,410 for PT and Speech combined, will increase to $2,480 for CY2026. Continued use of the KX modifier is required for all therapy services that “would have exceeded the previous therapy cap amounts,” or claims will be automatically denied.
The KX Modifier is an attestation by the therapist that the resident continues to require medically necessary services beyond the dollar threshold, and the rationale for the extended therapy services are documented in the medical record. All therapists should be aware of the amount of therapy a resident has received in a calendar year, and if over the threshold during a current episode of care, documentation should focus on supporting the extended services.
Manual Medical Review
The manual medical review threshold continues at the same amount of $3,000 until the next revision begins CY2028.
This type of review is not automatic when the $3,000 is reached. CMS uses the Targeted Probe and Educate (TPE) review process with providers identified through data submission as “outliers.” The TPE looks for providers with a high number of claim denials, questionable practice patterns including high number of units per day, and provides training to decrease the error rate. For more information on the TPE process, visit the CMS info page or check out the Q&A Document.
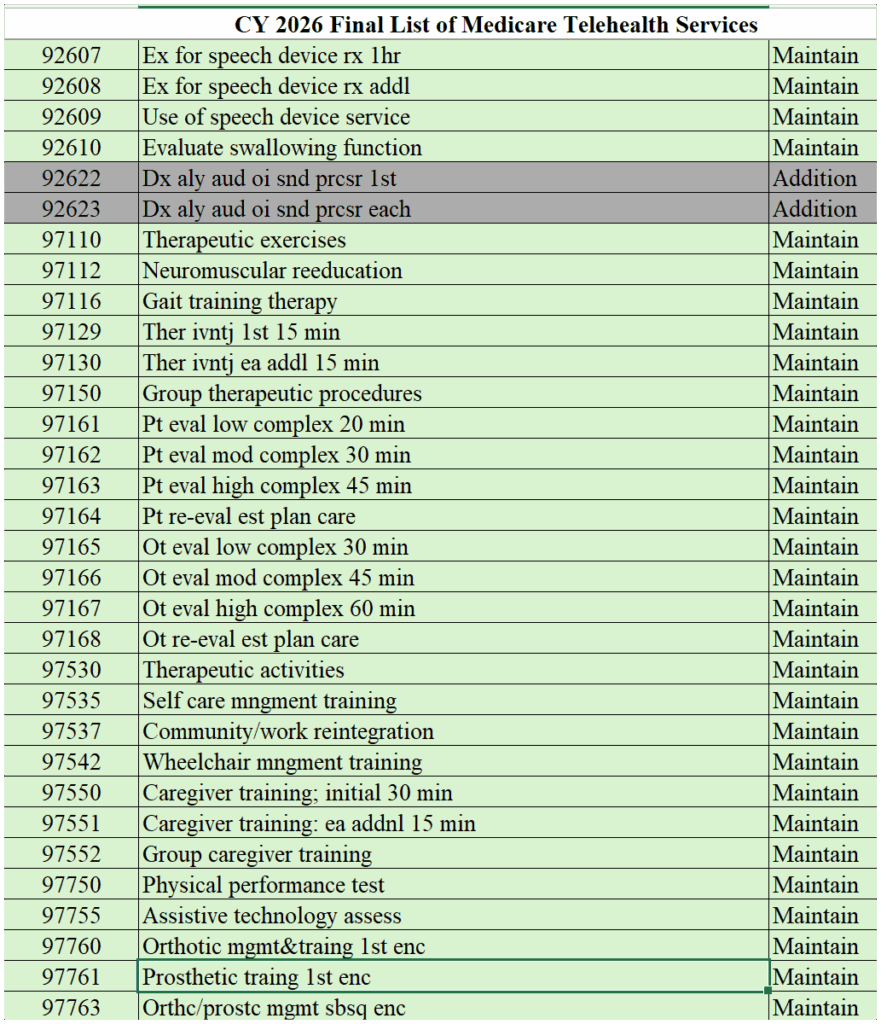
3. Telehealth
As we are all well aware, therapy professionals, by law, could not provide telehealth services prior to the Public Health Emergency (PHE) and were only able to provide telehealth post-PHE, through legislation that temporarily extended these flexibilities. This ability for therapy professionals was set to expire on 9/30/25 (unrelated to the Final Rule).
However, the temporary spending Bill passed on 11/12/25 to end the government shutdown included language extending the PHE telehealth flexibilities that allow therapy professionals to provide telehealth. This has now been extended until 1/30/26, and new legislation would be required at that time to allow therapists to continue.
The Final Rule included an updated list of Telehealth CPT Codes for CY2026. Below is the link to the list of acceptable codes, as well as a snapshot of the CPT Codes used in SNF therapy. Only codes from the list can be provided via telehealth. Additional audiology codes were added.
CY 2026 PFS Final Rule List of Telehealth Services
4. Changes to Therapy-Used CPT Codes
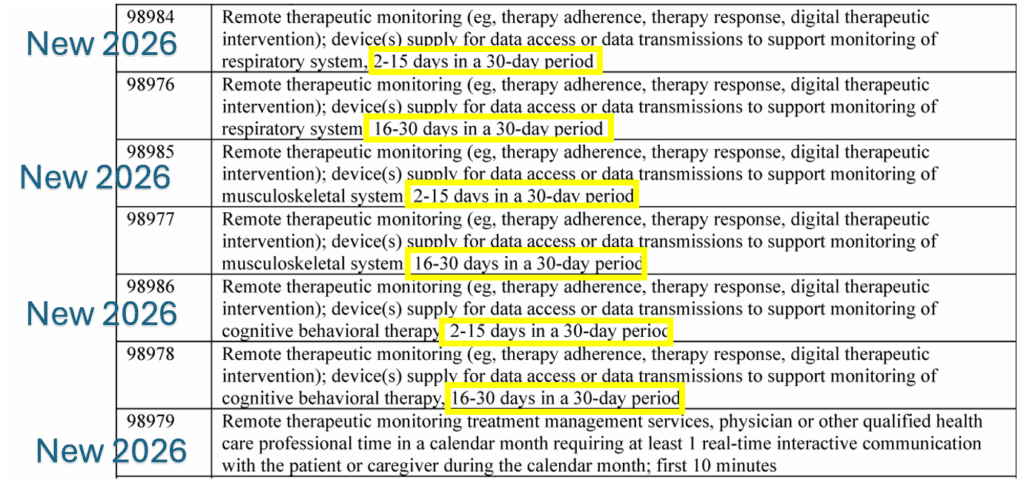
The Final Rule introduces 4 new Remote Therapeutic Monitoring (RTM) CPT Codes to be added to the current list of RTM Codes. The current CPT Codes represent monitoring a resident remotely 16-30 days in a 30-day period. The new Codes allow for billing of monitoring 2-15 days in a 30-day period.
The codes and descriptors can be seen below:
Important Links + Resources
Here are all the resources needed to dig deeper…
Final Rule – Federal Register Version | PDF Version
Corrected Final Rule Issued 11/28/25 – Link
Final Rule Home Page (Includes links to all tables)
In Summary
For CY2026, SNF Part B services can expect the 1st rate increase in years, an updated KX Modifier Threshold and a few new Remote Therapeutic Monitoring (RTM) CPT Codes. Not too bad for a change!
An added bonus, unrelated to the Final Rule, though coinciding with the Rule’s timing, is the ability for therapy professionals to continue to provide telehealth services through 1/30/26.
As always, if you have any questions about the information or how it will impact you, send them to us here: Just Ask Q&A
In Your Corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Resource Team
MonteroTherapyServices.com
