In the SNF setting, Rehab Managers, MDS Coordinators and Social Workers are among the staff designated to issue these “forms” to Medicare residents. All forms have a unique purpose and deadline for delivery. These “forms” include:
- Notice of Medicare Non-Coverage (NOMNC) – For Medicare Part A and B
- Detailed Explanation of Non-Coverage (DENC) – For Medicare Part A and B
- SNF Advanced Beneficiary Notice (SNFABN) – For Medicare Part A
- Advanced Beneficiary Notice of Non-Coverage (ABN CMS-R-131) – For Medicare Part B
Forms are updated periodically by CMS and released to providers. Dates listed on the bottom of each form can help providers track when forms expire.
Updated ABN Form for Medicare Part B
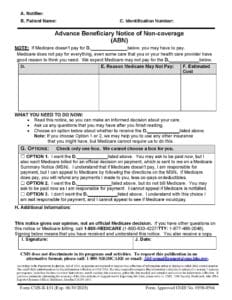
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, expired in March 2020. CMS has just issued a new form to take it’s place, effective on 8/31/2020. [Edit:On 8/4/20, CMS moved the due date to 1/1/2021] The CMS-R-131 is issued by providers to Medicare Part B beneficiaries in situations where Medicare payment is expected to be denied. The ABN is issued in order to transfer potential financial liability to the Medicare beneficiary in certain instances. Though there are no changes in content with the new form, SNF’s are required to provide the most updated form or financial penalty may result.
What do SNF’s need to do?
Print and/or Download the new CMS-R-131 form and begin using it now. Replace the form with a 3/2020 expiration date in the lower left corner. The new form has an expiration date of 6/30/2023.
Deadline for implementing the new CMS-R-131?
August 31st, 2020 Edit: On 8/4/20, CMS moved the due date to 1/1/2021
Where can SNF’s print the new form?
Where can SNF’s print the form instructions?
Why would a SNF issue this form?
The CMS-R-131 is issued in order to transfer financial liability to beneficiaries to convey that Medicare is not likely to provide coverage in a specific case. An example in the SNF would be if therapy deemed services no longer medically necessary, and the resident insisted on continuing services. The form would be issued only if therapy were to continue providing the services. The form outlines that Medicare will likely NOT pay for the service, and provides a cost estimate to the resident that he/she will be responsible for paying.
Image of the Updated Form
Guidelines for issuing the ABN can be found beginning in Section 50 in the Medicare Claims Processing Manual, 100-4, Chapter 30 (PDF).
*Please note that for residents with both Medicare and Medicaid, the form requires modification by the provider before giving it to the resident. Modifications include striking out Option 1 words “You may ask to be paid now but…also,” and “I understand that if Medicare doesn’t pay, I am responsible for payment, but I can appeal to Medicare by following the directions on the MSN.” Click the link HERE to access the instruction manual.
Submit any questions you may have through our Just Ask Q&A Forum and we would be happy to assist you!
If you would like more information on all SNF Beneficiary Notices, including scenarios, timelines for delivery, Medicare appeals, and the role of the SNF Rehab Manager in the process, check out our Webcast HERE (free for Facility Members) for 2 CE’s. We are a NYS approved provider of continuing education for therapy professionals.
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Rehab & MDS Compliance Team
*This article was edited on 8/5/20 to add the most recent CMS update: On 8/4/20, CMS moved the due date to 1/1/2021