
Centers for Medicare and Medicaid Services (CMS) released the Medicare Part A Skilled Nursing Facility (SNF) Prospective Payment System (PPS) FY2026 Proposed Rule containing the components that will go into effect 10/1/25 pending any changes made based on comments submitted to CMS over the next few months.
The information in this article is structured as a resource and teaching tool for SNF therapy and MDS professionals. The information is divided into the 3 main topics of the Rule tied to Medicare Part A and incorporates the pending changes for each:
- Part A Rates, PDPM and the MDS
- SNF Quality Reporting Program (SNF QRP)
- SNF Value Based Purchasing (SNF VBP)
A solid foundation in each of these areas will allow you to help your facility succeed. Take it 1 piece at a time….
Medicare Part A Rates, PDPM Changes & MDS Changes
Medicare Part A Rates
The Federal Per Diem rates are updated annually, and for Part A, we typically see an increase, unlike the Part B yearly therapy reductions. On 10/1/25, the rates for Part A have a proposed net increase of 2.8%, which equates to an overall increase in payment to SNFs in FY2026 of $997 million distributed between the 15,000+ SNFs today.
To put the proposed 2.8% increase in perspective, if all 15,000+ SNFs received equal “raises” this would equate to approximately $66,500 more this year, as compared to the 4.2% increase last year, or $87,000 more per SNF. Not quite the raise this year!
The details of how the 2.8% is derived can be found here:
- [(Market Basket increase of 3.0% + Forecast Error Correction of 0.6%) – 0.8% Productivity Adjustment (MFP)] = -2.8%.
Below are the proposed Unadjusted Federal Per Diem rates used to calculate each Patient Driven Payment Model (PDPM) Case Mix Group (CMG) rate.
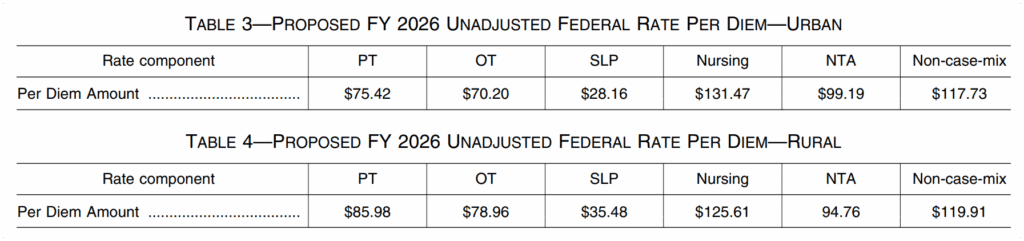
Now that we have daily per diem rate information, let’s put this together with changes to the Case Mix Index values in the next section to outline the individual rate for each Case Mix Group.
Medicare Part A PDPM Changes – Case Mix Index Values
Case Mix Index (CMI) values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, are updated annually as needed. These values are important as they assign “weight” to each of the CMGs, and when multiplied by the daily per diem rates in the prior section, determine the rate for each individual CMG.
The CMI values for each of the 5 components for 10/1/25 will remain the same as last year. The dollar values will be different, of course, due to the rate changes, but the CMI values will remain the same.
Here are the proposed “adjusted” daily rates for each of the case mix groups (CMG), derived by multiplying the Unadjusted Federal Per Diem Rate with the CMI value assigned to each CMG. These are the pieces needed in order to calculate the total daily rate.
Total Daily Rate = PT + OT + SLP + Nursing + NTA + Non-Case Mix Rate
The chart below shows the CMI values for each group and the resulting rate once multiplied by the Unadjusted Federal Per Diem Rates above.
Proposed FY2025 (Urban and Rural)
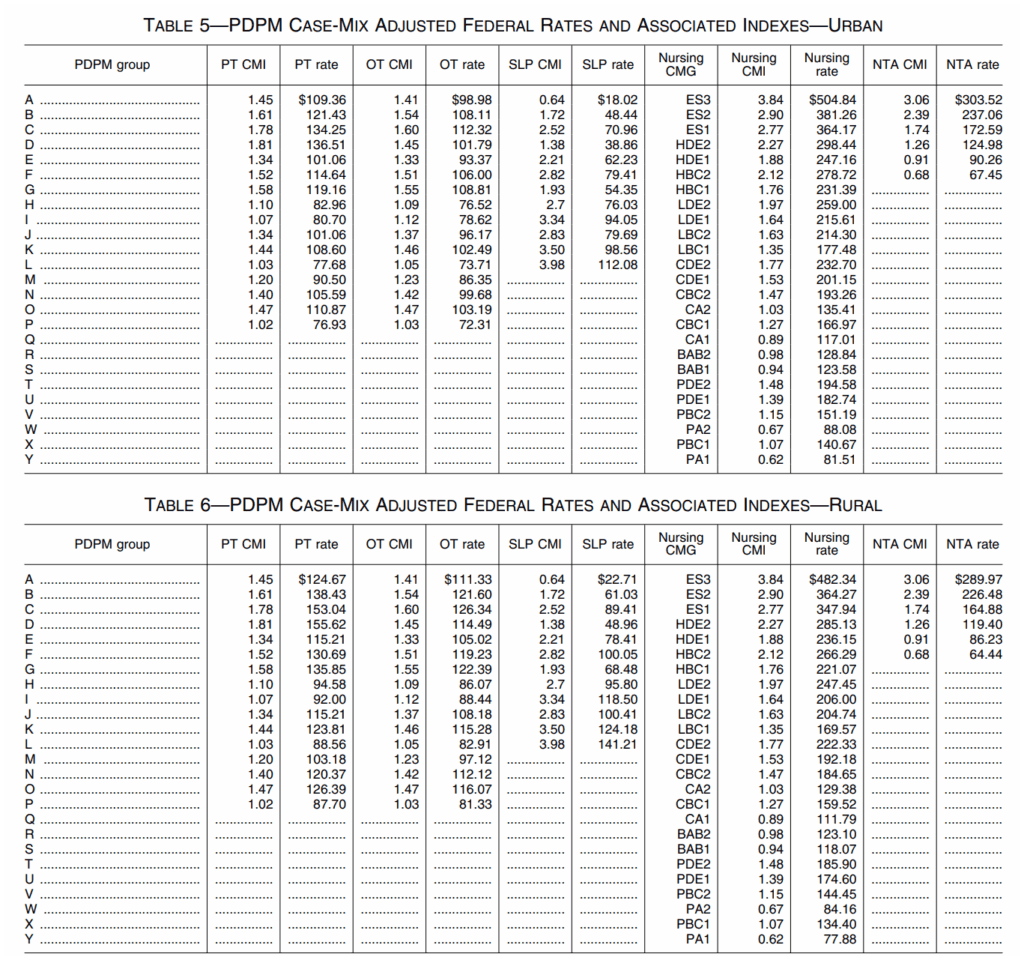
As a reminder, all of the CMG scores are derived based on how the MDS “trigger questions” are answered. The Non-Case Mix Group Rate is a “flat rate,” not tied to the MDS.
For example, using the Urban chart above, a HIPPS Code of KACD1 represents TK [PT $108.60] + TK [OT $102.49] + SA [SLP $18.02] + ES1 [Nursing $364.17] + ND [NTA$124.98] + Non-Case Mix Rate [$117.73]. The total base rate for this HIPPS Code would be $835.99 per day.
The total rate per day fluctuates based on what “PPS day” it is. Days 1-3 see a higher rate due to the NTA Component paying triple, and days 21-100 see a rate reduction as the PT and OT Components slowly decrease in value throughout the stay. The base rate reflects payment for days 4-20, when there are no variables that impact the rate involved.
Changes In Wage Index – Geographical Locations – For part a rate calculation
In the section above, we demonstrated how to calculate the daily per diem rate. To take this rate and transform it into the rate that your SNF will receive, requires another piece of the puzzle…. the Wage Index (WI).
CMS categorizes SNFs as Urban or Rural and assigns a unique WI value to each county or state. This WI is a variable used to take the Total Daily Per Diem Rate and adjust it up or down based on where you live.
The total daily rate explained in the section above is comprised of a Labor Portion and a Non-Labor Portion. The WI is used to adjust the Labor Portion to get your location-specific rate.
Total Daily Rate = Labor Portion + Non-Labor Portion
Your SNFs Total Daily Rate = (Labor Portion x Your SNFs Wage Index) + Non-Labor Portion
CMS updates these WI values each year. The proposed Wage Index Tables for FY 2026 can be found here:
Make note of whether your SNF is Urban or Rural, and your area WI. Not sure if your SNF is classified as urban or rural? Use the Wage Index Look Up Tool HERE and plug that into the PDPM Calculator to get your rates.
Medicare Part A PDPM Changes: ICD-10 Code Mapping For PT, OT + Speech Components
The ICD-10 Code selected for MDS Section I0020B as the primary reason for SNF Part A covered care is used for case mix classification under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, or identified as a Return to Provider (RTP) code.
In other words, Return to Provider Codes can’t be used to represent the primary reason for skilled care in Section I0020B, and the code that is used in this Section will fall into 1 of the 4 collapsed Clinical Categories below, thus, determining the PT/OT Component grouping.
It is important to note, Section I0020B is the only place where RTP codes can’t be used. RTP simply means “the diagnosis is not valid to represent the primary reason for a Part A stay.” These RTP codes can be placed in Section I8000 of the MDS or on the billing claim if they accurately represent an active diagnosis for the resident.
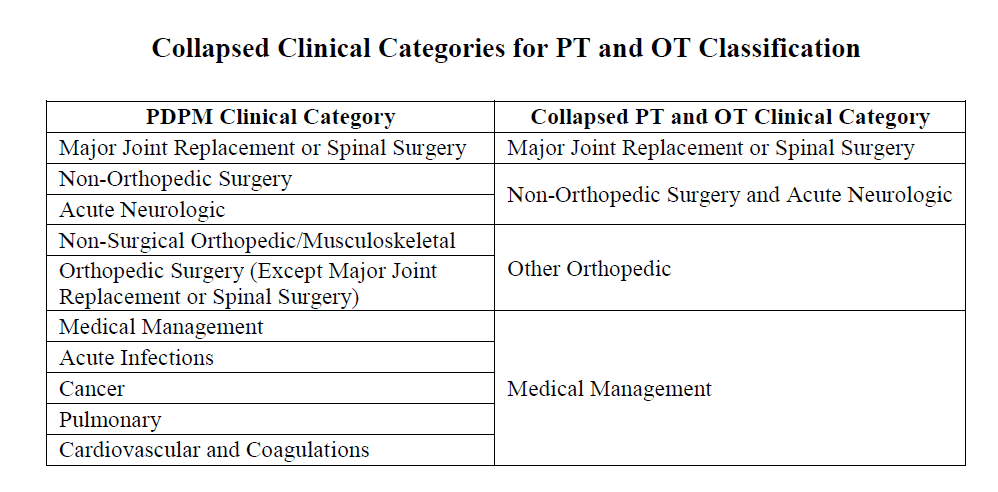
Each year, CMS makes modifications to the mapping of certain ICD-10 Codes. This year, CMS is proposing to change the clinical category assignment for the following thirty-four ICD–10 codes that were new to PDPM in 2024.
Mapping is Changing from Medical Management to Return to Provider (33)
- E10.A0 (Type 1 diabetes mellitus, pre-symptomatic, unspecified),
- E10.A1 (Type 1 diabetes mellitus, pre-symptomatic, Stage 1)
- E10.A2 (Type 1 diabetes mellitus, pre-symptomatic, Stage 2)
- E10.9 (Type 1 diabetes mellitus without complications)
- E16.A1 (Hypoglycemia level 1)
- E16.A2 (Hypoglycemia level 2)
- E16.A3 (Hypoglycemia level 3)
- E16.0 (Drug induced hypoglycemia without coma)
- E16.1 (Other hypoglycemia)
- E16.2 (Hypoglycemia, unspecified)
- E16.3 (Increased secretion of glucagon)
- E16.4 (Increased secretion of gastrin)
- E16.8 (Other specified disorders of pancreatic internal secretion)
- E16.9 (Disorder of pancreatic internal secretion, unspecified)
- E66.811 (Obesity, class 1)
- E66.812 (Obesity, class 2)
- E66.89 (Other obesity not elsewhere classified)
- E66.01 (Morbid (severe) obesity due to excess calories)
- E66.09 (Other obesity due to excess calories)
- E66.1 (Drug induced obesity)
- E66.3 (Overweight)
- E66.9 (Obesity, unspecified)
- F50.010 (Anorexia nervosa, restricting type, mild)
- F50.020 (Anorexia nervosa, binge eating/purging type, mild)
- F50.021 (Anorexia nervosa, binge eating/purging type, moderate)
- F50.21 (Bulimia nervosa, mild)
- F50.22 (Bulimia nervosa, moderate)
- F50.810 (Binge eating disorder, mild)
- F50.81 (Binge eating disorder, moderate)
- F50.83 (Pica in adults)
- F50.84 (Rumination disorder in adults)
- F98.21 (Rumination disorder of infancy and childhood)
- F98.3 (Pica of infancy and childhood)
Mapping is Changing from Acute Neurologic to Medical Management (1)
- G90.81 (Serotonin syndrome)
Below is the new DRAFT ICD-10 Mapping File for all PDPM ICD-10 Mapping. The mapping files are needed to determine the Case Mix Group for the PT/OT, Speech and NTA Components. Your EMR may have some of this information built in, however, using the source documents from CMS is your best bet.
Changes to the Non-Therapy Ancillary (NTA) Component
Potential changes to the NTA Component were the highlight of the Proposed and Final Rules last year. In those Rules, CMS solicited information about potential future NTA changes, and gave examples of what the NTA Component may look like in future Rules.
This year’s Rule….. crickets.
Let’s hope no news is good news for now.
If you are interested in the potential NTA changes CMS discussed, we explained them in detail in our review last year.
mDS Changes Coming 10/1/25
The Draft RAI Manual and the Draft Item Sets for 10/1/25 have been released.
Here is the link to the updated Draft RAI Manual. All items in red identify what’s new. The best way to familiarize yourself with the changes (assuming you were familiar with the Manual before the changes) is to scroll and read all the “red” and then go to the end of the Manual and look at all the track changes where you can see what was added and crossed out for each section.
Draft_MDS-3.0-RAI-Manual-v1.20.1_October_2025 (1) (PDF)
Draft Item Set Links below:
- Comprehensive (Admission, Annual, Significant Change)
- 5-Day PPS
- For all others, visit our MDS 3.0 Toolbox
There are some minor changes scattered throughout the Draft Manual, as well as a major change for Section O: Therapy Days and Minutes.
Let’s start with the minor changes.
- A0800 & X0300 Gender removed and replaced with A0810 & X0310 Sex on all assessments
- A1250 Transportation was removed and is now in new “Section R”
- A2000 Discharge Date was removed from the End of PPS MDS
- A2400 Medicare Stay No/Yes change in skip pattern for End of PPS MDS
- B0100 Comatose change in skip pattern based on answer for End of PPS MDS
- I7900 Active Diagnoses “None of the Above” added to Quarterly, OBRA DC, 5 Day
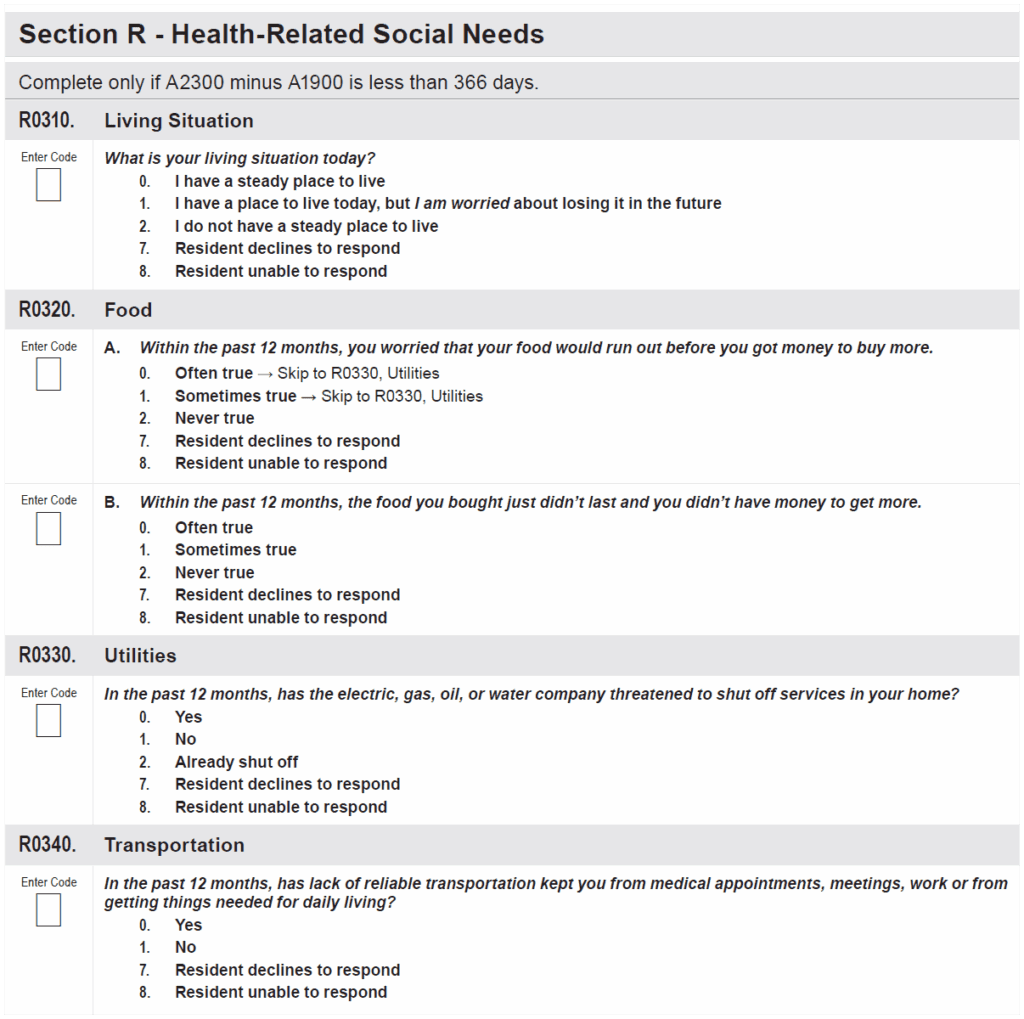
- New Section R Social Determinants of Health questions added to PPS 5-Day for residents admitted less than 366 days prior. Though the questions remain, per the Proposed Rule, they will no longer be tied to the SNF QRP (No penalty for dashing…more on this in the SNF QRP Section Below). FYI Transportation is not new, it migrated here from Section A.
Here are the new data elements / questions in Section R:
Now for the major changes. Section O: Therapies
Section O0400, “Therapies,” which includes data collection for Physical, Occupational and Speech Therapy, as well as Respiratory, Psychological and Recreational Therapy, will be removed from all MDSs, with the exception of Item O0400D2 “Respiratory Therapy Days,” which is needed for PDPM HIPPS Code calculations. Section O0420 Distinct Calendar Days of Therapy will also be removed for all non-Medicare Part A resident assessments.
Section O0400 includes items all to familiar for therapists such as Therapy Start Date, Therapy End Date, Type or Mode of Therapy (Individual, Group, Concurrent, Co-treatment), Total Days and Total Minutes. Mind you, this is a veteran section, that has been on the MDS for decades.
We were teased with this change in October 2023, when the accidental? removal of these items occurred in conjunction with the MDS overhaul at that time (when GG replaced G….). However, CMS added the collection of these items back later that year. You can find the details in this meltdown article, “Is It Really Bye-Bye Therapy”.
How will therapy service detail be monitored going forward?
Section O0425: Part A Therapies will remain “as is” for Medicare Part A data collecting, and will continue to collect total Therapy Days and Minutes (including Individual, Concurrent, Group and Co-treatment). Section O0430: Distinct Calendar Days of Part A Therapy will also remain, and together, this information will calculate the amount and type of therapy provided over the course of a Part A stay, and will be used to track the % of Group and Concurrent services to monitor SNFs over the 25% threshold.
It is important to point out that this level of detail will be collected by CMS for Medicare Part A residents only….. for all other residents, which are the majority in the SNF setting, the details about therapy delivery, going forward, will need to come from your in-house or contract therapy group.
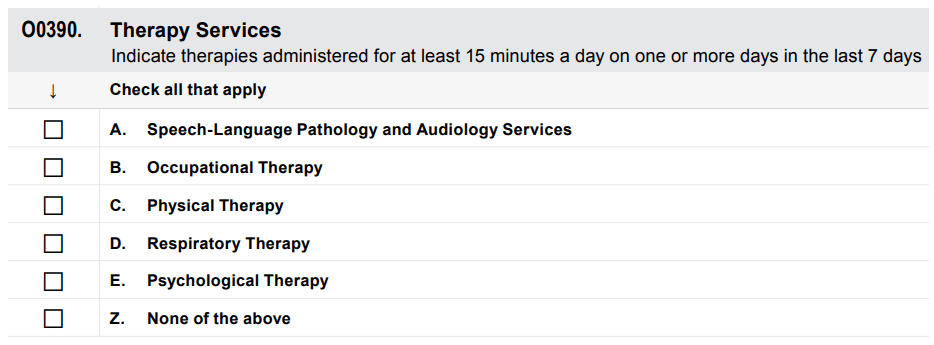
A new question [O0390] has been added to the OBRA Admission, Quarterly, Annual, Significant Change and the PPS 5-Day to indicate [via a “check mark”] when any of the therapy services have been provided for at least 15 minutes on any 1 day during the 7-day look-back window. This new item will only tell us if therapy was provided, and does not give real usable information in terms of frequency and intensity.
In last year’s Final Rule, CMS responded to the multiple comments submitted identifying concern with removing these items. CMS indicated these MDS items are not needed to determine PDPM payment, and removal of the items decreases the “burden” on those completing the MDS by “6.6 minutes.” CMS acknowledged the reduction of therapy service volume and intensity since the start of PDPM, though reiterated that the impact on resident function is the bottom line, and Measures are in place to monitor this.
The new question looks like this:
Before we move on, let’s take a moment of silence to remember Recreational Therapy, as they did not “make the cut” to transition to the updated section with the other “therapies,” and will no longer be on the MDS.
we see you
Moving forward….
Changes To CMS Medicare Part A Quality Measure Programs
If you are not already heavily involved in your SNF Quality Measure Program processes, NOW is the time. As these Measure Programs grow and grow, don’t get left behind. By understanding the Measures and Programs, SNF therapy and MDS professionals can be a godsend to their facility. Here, we break down each program and what will be changing.
SNF Quality Reporting Program – SNF QRP
The SNF QRP is the program that started small over 9 years ago [remember when Section GG was new?] and has now ballooned into the program with the most measures. This is a pay for reporting program, meaning, SNFs are required to report measure data on specific MDS items, and if not reported, facilities can be subject to a 2% Part A payment penalty.
The penalty occurs when information is missing, not for poor outcomes. [yet]
Here is a link to all the MDS questions that, if not filled out, will trigger the payment penalty if the threshold is met. This list is in effect for Q4 2025. CMS will release the FY2028 table soon.
The list of item sets (MDS questions) continues to grow, making the attainment of submitting 100% of the required quality measure data collected on at least 90% of all PPS Part A assessments to void the penalty is a challenge!
Make sure MDS staff have the list of MDS items above. These are the MDS items being collected NOW that will potentially impact FY 2027 & 2028 Annual Payment Update (APU) Determination.
The SNF QRP works in 2 time tables. The collection of data NOW [reporting period] will impact your payment in the FUTURE.
In addition to submitting 90% of all Part A MDS assessments with no missing data, SNFs also need to submit 100% of data for the COVID-19 and Influenza Vaccination for Healthcare Personnel to the CDC National Healthcare Safety Network (NHSN). If info is missing on the MDS or vaccination info is not sent timely to the CDC, the penalty will apply. This does not leave much room for error.
SNF QRP Changes for FY2026
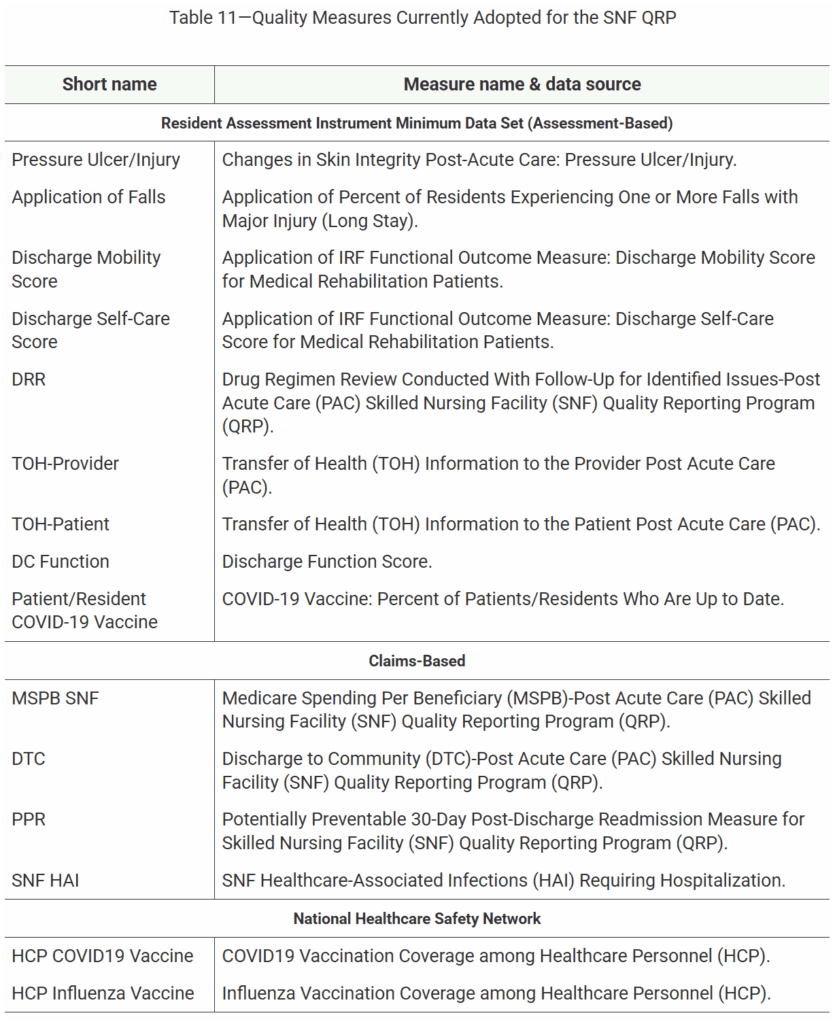
There are no “new Measures” for the SNF QRP in the Proposed Rule. But that does not mean we can sit back and relax. Below are the 15 current Measures in place for 10/1/25 (FY2026). The 1st 9 are solely dependent on how the MDS questions are answered.
Easy Come, Easy Go
Last year, CMS finalized the addition of 4 new item sets / MDS questions, or standardized patient assessment data elements (SPADES) in the Social Determinants of Heath (SDOH) category, that would correlate to the SNF QRP program, as well as the potential Part A “penalty” for not answering the questions.
The 4 new questions (Living Situation, Food, Utilities) are detailed above in the MDS Changes section as they will make their debut on the MDS 10/1/25. Data collection for these items for PPS residents in the SNF < 366 days will begin 10/1/25, though per the Proposed Rule, these 4 items will no longer have a payment impact in FY2027, and will be removed from the SNF QRP. CMS stated “we acknowledge the burden associated with these items at this time….and look for ways to balance the need for data collections regarding quality care and burden of these data collections on health care providers.” CMS will work towards a better way to capture this data going forward.
In other words, at this point, we will have these 4 new questions on the MDS but they will not count toward a payment penalty if we “dash” them for Part A residents. It is possible that the 4 items may be removed from the MDS with future updates.
Other SNF QRP Changes
The Proposed Rule outlines additional changes to the Reconsideration Policy and Process. The Reconsideration Process is when SNFs are not in agreement that they did not comply with reporting requirements, and are notified of a pending 2% payment penalty for their SNF.
The Proposed Rule includes 2 new items in this area:
- Allowing SNFs to Request and Extension to File for Reconsideration based on extraordinary circumstances (natural disaster, etc.)
- Modifying existing reconsideration policy to provide that CMS will grant a timely request and reversal
Future SNF QRP Measures
In the Proposed Rule, CMS is seeking comments, or Requests for Information (RFI) in 3 areas. This information is used to solicit feedback for future rule making:
- Future measure concepts for: Interoperability, Well-being, Nutrition and Delirium
- Potential revision to the data submission deadlines for assessment data collected for the SNF QRP from 4.5 months to 45 days, with the goals of having more current data available to the public to make informed decisions on where to receive care, as well as providing data to SNFs for their quality improvement efforts sooner. Currently, there is a 9-month lag of presented data.
- Advancing digital quality measurement in the SNF – Seeking feedback on the current state of health information technology in the SNF setting
On to the last Quality Measure Program….
SNF Value-Based Purchasing Program (SNF VBP)
The SNF VPB Program is a “pay for performance” program and works by withholding 2% of all SNFs’ Medicare Part A payments to fund the program, and then allows for an opportunity for SNFs to recoup part of the 2% by demonstrating “success” with the established Measures. CMS redistributes approximately 60% of this back to SNFs as “incentive payments” to encourage improvements in the quality of care provided to Medicare beneficiaries (and yes, CMS keeps the remaining 40%).
Current SNF VBP Measures
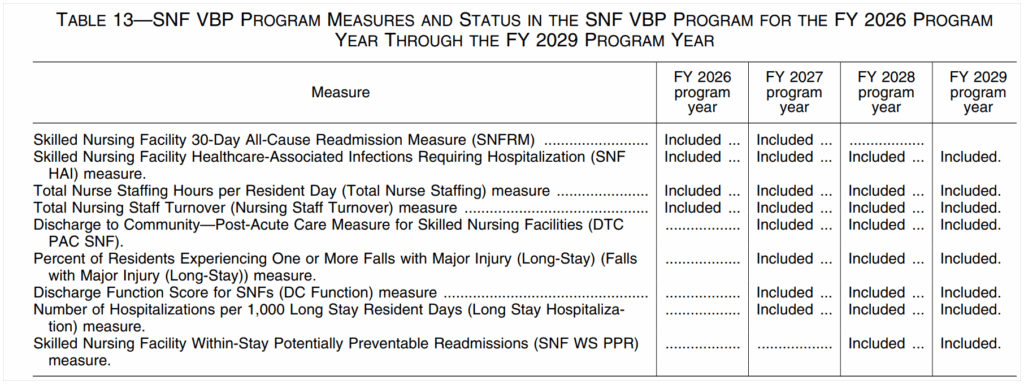
Though there are no new measures in this year’s Proposed Rule, we are all impacted by the multitude of new measures added over the past few years that are slowly kicking in.
Since the start of this Program, there has only been 1 Measure: The SNF 30-Day-All-Cause Readmission Measure, which looks at residents readmitted back to the hospital within 30 days of entering the SNF from the hospital. However, 10/1/25 marks the FY2026 Program Year where 3 additional Measures will have a payment impact.
The timeline of all the VBP Measures are listed below.
It is important to note that the Program Year is synonymous with “payment impact year,” which follows 2 years after the “Performance Year. So even though some of these dates feel a bit “far off,” we need to pay attention to the Performance Year, as this is the “data collection start date.”
Once the Program Year hits, it’s too late to do anything about the data.
- The 4 Measures in the FY2026 Program Year will impact the SNF score and payment on 10/1/25 from data that was collected in FY2024.
- The additional 4 Measures in the FY2027 Program Year will impact the SNF score and payment on 10/1/26 based on data collected in FY2025 (now). This includes Discharge to Community, Falls with Major Injury, Discharge Function Score and Hospitalizations per 1000 Long Stay Resident Days.
Jumping ahead…..data collection for the FY2028 Program Year Measures will begin FY2026, or 10/1/25.
SNF VBP Measure Performance Standards
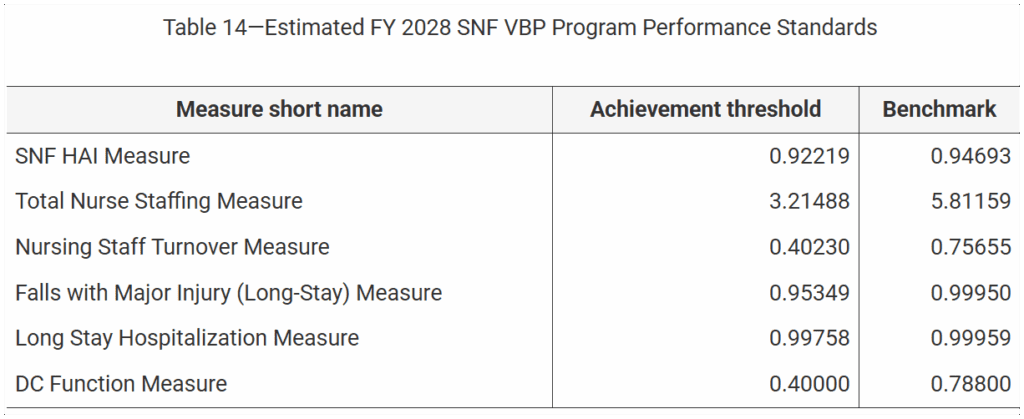
The Proposed Rule released the Achievement Threshold and Benchmark for each of the VBP Measures as shown below.
other sNF VBP changes
Change in Scoring Methodology
CMS proposes removing the Health Equity Adjustment (HEA) that was supposed to kick in 10/1/25, before it had a chance to start. The HEA was set to reward top tier performing SNFs that served higher proportions of dual eligible residents (Medicare/Medicaid). Removing the HEA avoids a change in the variable payback rate and will maintain the 60% payback method that SNFs have been accustomed to since 2022. CMS contributes the removal of the HEA to program simplicity and regulation streamlining.
Adopting a Reconsideration Process
CMS proposes to adopt a reconsideration process that will allow SNFs to seek reconsideration of a “review and correction” request if they are not satisfied with the CMS decision. This process would provide SNFs an opportunity to review information that is to be made public prior to publication.
What’s Next?
CMS is accepting comments for the Proposed Rule through June 30, 2025. Comments are reviewed and used to determine if changes will be made in the Final Rule due out this summer. Electronic comments can be made at https://www.regulations.gov Follow the “Submit a comment” instructions.
Additional Resources to Do Your Own Homework
HERE is a link to the Proposed Rule PDF Version
HERE is a link to the Federal Register Proposed Rule
HERE is a link to the CMS Fact Sheet
PDPM Calculators and Resources HERE
If you have any questions, send them to our Just Ask Q&A Team and we will get your questions answered.
Thank you for all you are doing to provide the best care to the geriatric population!
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
President | Montero Therapy & MDS Resource Team
MonteroTherapyServices.com
