Respiratory Therapy (RT) is not new to the skilled nursing facility (SNF) setting or new to the Minimum Data Set (MDS). The data for RT has been coded in Section O of the MDS for years, generating a Special Care High Nursing score…the second highest possible nursing category…and…the rules for RT have not changed.
So why has Respiratory Therapy been getting so much attention lately?
Since the implementation of the Patient Driven Payment Model (PDPM) in 2019, interest in initiating RT programs in SNFs that do not have ventilators or residents that require tracheostomy care has spiked. Why? Under the prior Medicare Part A payment system, RUG scores would case mix maximize, meaning that even if the resident met the qualifiers for RT, it would not be reflected in the RUG score or reimbursement rate when a higher RUG score was achieved. In essence, residents scoring in a Rehab Ultra RUG {and some RV and RH RUG groups} would receive the same reimbursement whether that resident was receiving RT or not.
Under the new PDPM structure, SNFs are reimbursed for the Nursing Component independently of all other components, including Therapy. Therefore, residents receiving RT have a higher Nursing Case Mix Group and overall higher daily reimbursement rate as compared to residents not receiving RT.
So now, SNFs are asking questions such as…
- What does the reimbursement for RT look like?
- How many days per week is RT needed for capture?
- Can RT be provided by nursing staff? Physical Therapy?
- Is a physician order needed?
- What needs to be documented to capture RT?
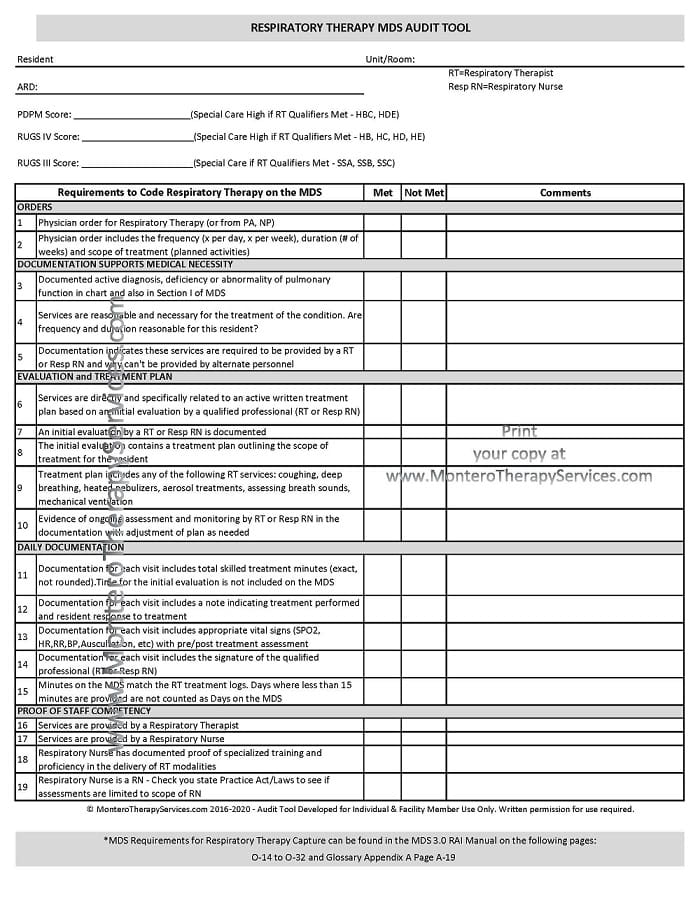
We thought we would help you breathe easy by answering some of those questions & sharing an audit tool that may come in handy if you are looking for a way to self-audit, or if you are thinking about implementing a program and need a place to start.
SNF Respiratory Therapy Qualifiers
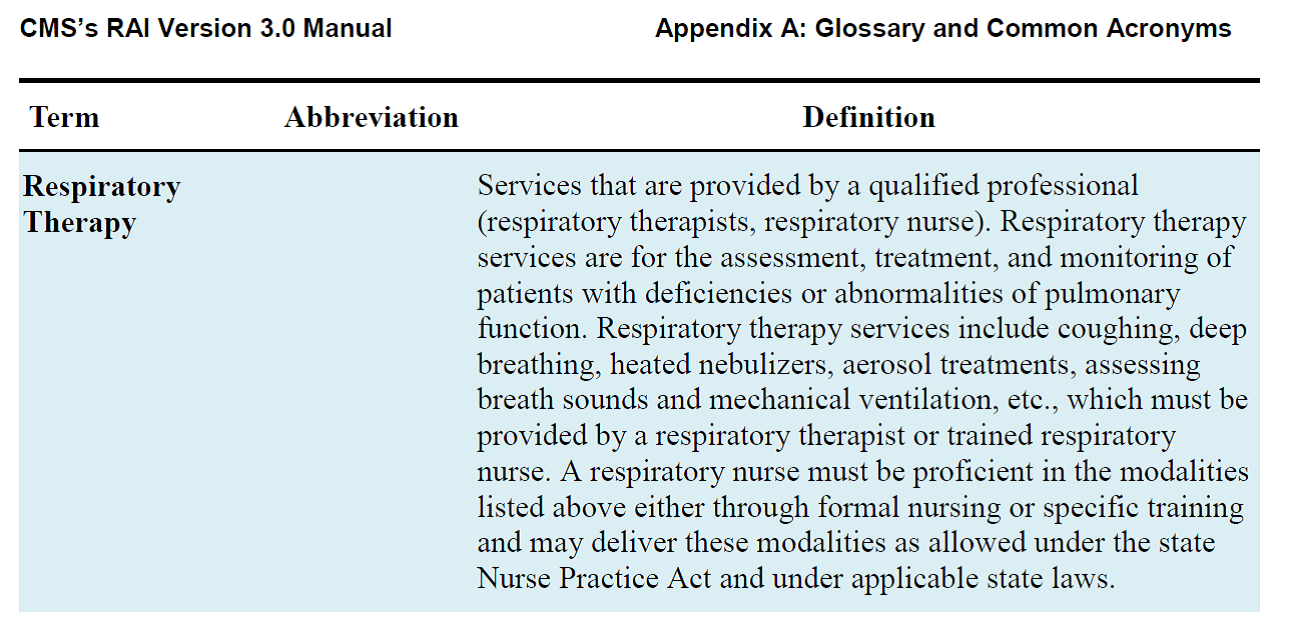
The RAI Manual defines Respiratory Therapy as “skilled services for the assessment, treatment and monitoring of those with deficiencies or abnormalities of pulmonary function. Treatments may include:
- coughing
- deep breathing
- assessing breath sounds
- heated nebulizers
- aerosol treatments
- mechanical ventilation
and are considered if provided by a qualified professional…” The Manual defines qualified professional as “a respiratory therapist and/or respiratory nurse.”
Here is the excerpt from Appendix A of the RAI Manual:
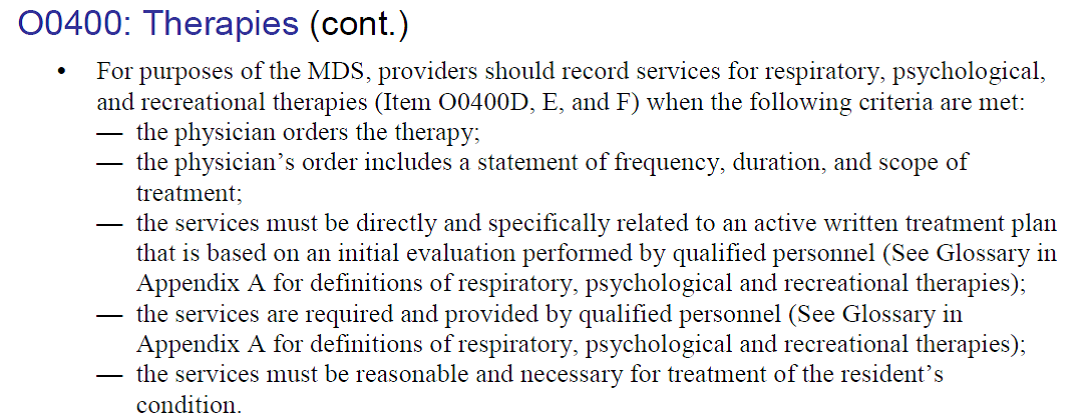
Section O0400 of the RAI Manual / Chapter 3, lists the criteria that must be met for coding respiratory therapy services on the MDS. Respiratory Therapy criteria models the criteria for physical, occupational and speech therapy, including:
- physician order that includes the frequency, duration and scope of treatment
- initial evaluation with treatment plan written by RT or respiratory nurse
- services provided by RT or trained respiratory nurse
- services must be reasonable and necessary for the resident’s condition
- services must be care planned and periodically evaluated to ensure that the resident receives needed therapies and that current treatment plans are effective.
Here is the excerpt from Section O: Page O-20 [Link to RAI Manual]
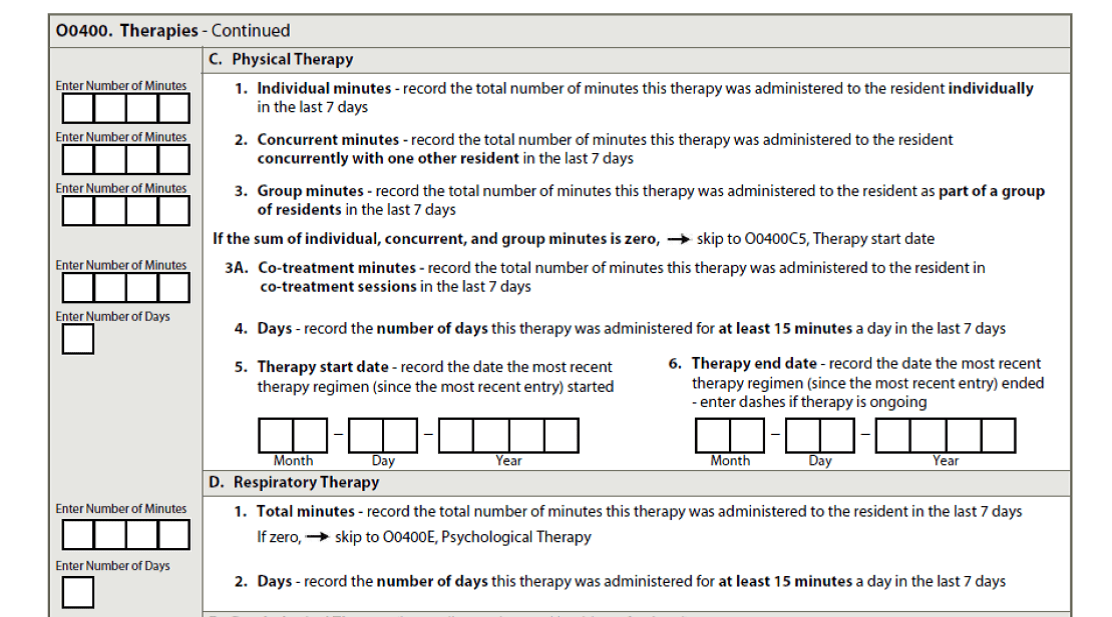
Recording Respiratory Therapy on the MDS in Section O0400 requires looking at the 7 day look back and listing the Total Number of Days (of at least 15 minutes of RT) and the Total Number of Minutes. All 7 days, with a minimum of 15 minutes each day, are needed to qualify.
Additional qualifiers include:
- Coding minutes that the respiratory therapist or respiratory nurse spends with the resident
- Coding time for evaluation, assessment, treatment administration, monitoring, setup and removal of equipment
- Excluding time that a resident self-administers a nebulizer treatment without supervision of the RT or Respiratory Nurse.
- Excluding time to administer metered-dose and/or dry powder inhalers
Respiratory Therapy Capture and Scoring
If the qualifiers are met and the Respiratory Therapy services are coded properly, the resulting scores will be as follows:
- PDPM: Special Care High with Case Mix Groups: HDE2, HDE1, HBC2 and HBC1
- As long as Nursing Function Score is <=14
- RUG-IV: Special Care High with RUG Groups: HB1, HB2, HC1, HC2, HD1, HD2, HE1 and HE2
- As long as ADL Score is >=2
- RUG-III: Special Care with RUG Groups: SSA, SSB or SSC
- Some states still use RUG-III for State Medicaid Case Mix.
Audit Tool
This audit tool breaks down the requirements into categories and will help walk you through what is needed to code Respiratory Therapy on the MDS. It is important to note that each State Practice Act defines the role of the RN and LPN, and some states by statute may disqualify LPN’s from “counting” as a “trained respiratory nurse” based on the assessment component needed to qualify for respiratory therapy – assessment of lung sounds, etc. State specific information is not included in the RAI Manual and must be obtained from each State Board.
Take a look at the Audit Tool below. Members can download the audit tool here.
If you have any questions, send them to our JustAsk Q&A Forum and we will be glad to help!
As Always….In Your Corner,
Dolores and the Montero Therapy Team
Rehab and MDS Compliance Professionals
www.MonteroTherapyServices.com