*Information accurate as of 3/26/20. It is anticipated updates from CMS will occur regularly over the next few weeks.
**CMS released the Interim Final Rule on 3/30/20. To access the Rule CLICK HERE . The Rule confirmed the information in this article regarding e-visits for private practice therapists. The Rule ADDED the authorization for private practice therapists to utilize Virtual Check-Ins (see chart below). The Rule also ADDED the temporary authorization for private practice therapists to use Telephone Evaluation and Management Services CPT codes 98966-98968. These are assessment and management services performed by practitioners who cannot separately bill for E/Ms. Please refer to page 122 of the Rule for details. Regarding Telehealth, the Rule also ADDED 97000 series CPT codes commonly used by therapists….HOWEVER, the Rule continues to confirm that therapists are not “approved providers” or ” approved distant site practitioners” and therefore, cannot bill Telehealth services at this time.
If you are a SNF therapy professional and have been trying to keep up with all the releases from the Department of Health and Human Services (HHS), Center for Medicare and Medicaid (CMS), Office of Inspector General (OIG), the President, your Governor, private insurance companies, APTA, AOTA, and ASHA, you may likely feel defeated.
This IS NOT our fist rodeo, but it IS our first pandemic…so let’s piece together the information you need to continue to provide therapy services {or decide not to} to the best of your abilities. With all of the resources and links in 1 place, finding the necessary information will be much easier. With that said, this has been a very fluid situation for the past 2 weeks and this may continue to be the case on both a Federal and State level, so use the resources here as a starting point on your search for specific information. Anticipate additional regulatory changes in the days to come.
Let’s review what we know to date has changed for Medicare Part A and Medicare Part B due to the COVID-19 National Emergency. This is a ton of information…you don’t need to digest it all now. Take 1 bite at a time.
First, Are You Essential?
SNF therapy status of essential or non-essential should not be defined or determined by your revenue-generating capability…just stating the obvious here. These terms refer to the “situation at hand.” Is your position essential or non-essential to the current situation in your location and/or place of employment?
Your employer may determine if your services are deemed essential. However, formal guidelines were provided by the Federal Government for the current National Emergency. The document below, developed by the U.S. Department of Homeland Security Cybersecurity & Infrastructure Security Agency (CISA) identifies “Essential Critical Infrastructure Workers,” and was developed to help State and local officials as they work to protect their communities, while ensuring continuity of functions critical to public health and safety, as well as economic and national security. CISA includes the following as essential: physicians, dentists, psychologists, mid-level practitioners, nurses and assistants, infection control and quality assurance personnel, pharmacists, physical and occupational therapists and assistants, social workers, speech pathologists and diagnostic and therapeutic technicians and technologists.
CLICK HERE to view the full document.
The Federal Document acknowledges that States will have the authority to make the ultimate decisions based on current condition, stating:
“We recognize that State, local, tribal, and territorial governments are ultimately in charge of implementing and executing response activities in communities under their jurisdiction, while the Federal Government is in a supporting role. As State and local communities consider COVID-19-related restrictions, CISA is offering this list to assist prioritizing activities related to continuity of operations and incident response, including the appropriate movement of critical infrastructure workers within and between jurisdictions. Accordingly, this list is advisory in nature. It is not, nor should it be considered to be, a federal directive or standard in and of itself.”
In addition to the Federal guidelines, each State may issue additional guidance. Check your state website to see if your Governor has issued guidance.
Information released by the Governor of New York, for example, does not specifically include therapy professionals, though does reference skilled nursing facility services as essential.
“For the purposes of this guidance, essential services are considered as Hospitals, Clinics, Emergency Medical Services, Residential Health Care Facilities, such as Nursing Homes…”
With that said, the Governor of New York has reached out to all licensed health professionals, including therapists, to ask for assist in managing the current State of Emergency in any way possible.
CLICK HERE for New York documents
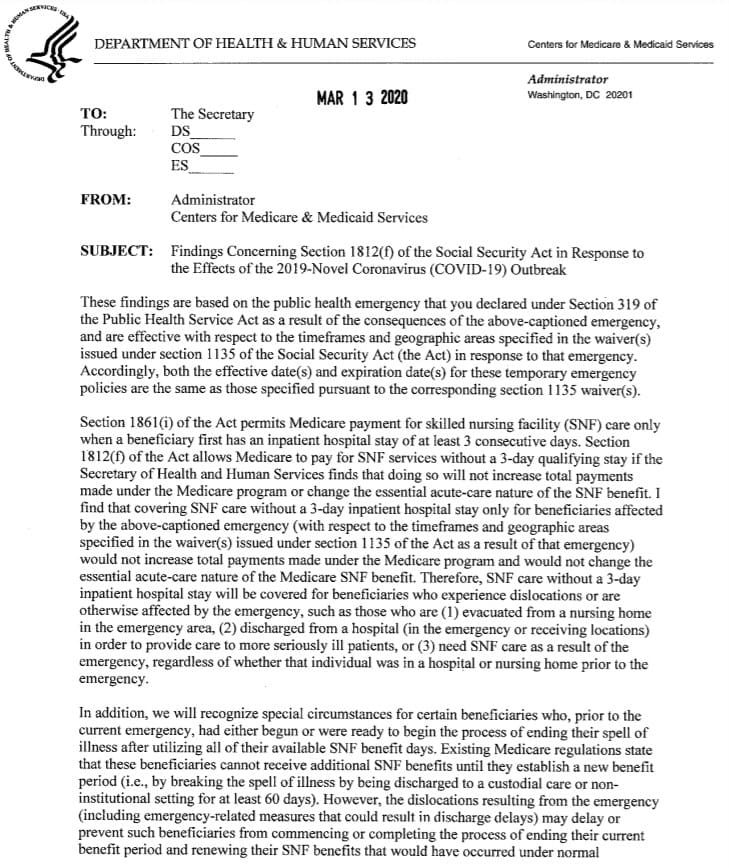
The Waiver
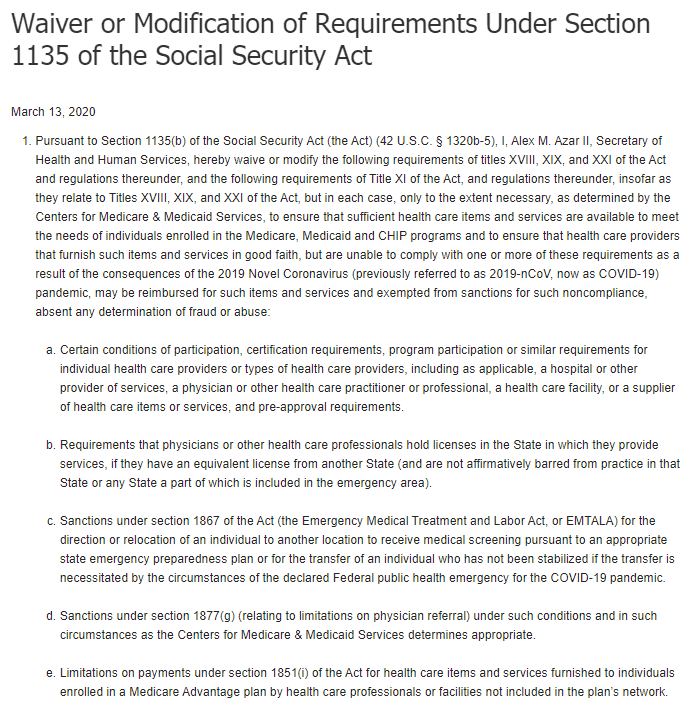
When the President declares a disaster or emergency under the Stafford Act or National Emergencies Act and the HHS Secretary declares a public health emergency under Section 319 of the Public Health Service Act, the Secretary is authorized to take certain actions. For example, under section 1135 of the Social Security Act, the Secretary may temporarily waive or modify certain Medicare, Medicaid, and Children’s Health Insurance Program requirements to ensure that sufficient health care items and services are available to meet the needs of individuals enrolled in Social Security Act programs in the emergency area and time periods and that providers who provide such services in good faith can be reimbursed and exempted from sanctions.
A National Emergency has been declared and the HHS Secretary has declared a public health emergency.
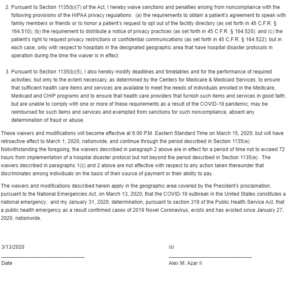
On March 13th, the Secretary of HHS signed a Waiver to modify requirements under Section 1135 of the Social Security Act. This 1135 Waiver has implications for both Medicare Part A and Part B. A copy of the Waiver is pictured below. CLICK HERE for the link to the Waiver on the HHS website.
Waiver 1135 is Federal and automatically applies to all States regarding Medicare.
However, individual States must apply for the Waiver for Medicaid benefits. CLICK HERE to see if your State has applied. This list is kept current by Medicaid.gov found HERE.
These waivers under section 1135 of the Social Security Act typically end no later than the termination of the emergency period, or 60 days from the date the waiver or modification is first published unless the Secretary of HHS extends the waiver by notice for additional periods of up to 60 days, up to the end of the emergency period.
Additional Important Waiver Resources
COVID-19 Emergency Declaration Fact Sheet for Providers
CMS MLN Matters – Released 3/20/20
1135 Waiver General Information
1135 Q&A Document – SNF Page 39
Waiver 1135 Impact on Medicare Part A in the SNF
On March 13th, the Administrator for CMS, Seema Verma, issued a letter to the Secretary of HHS to utilize authority under section 1812(f) to accomplish 2 things for Medicare residents of skilled nursing facilities impacted by the emergency:
- Temporarily change the 3-day hospital stay requirement to initiate SNF Medicare Part A coverage
- Temporarily change the 60-day spell of wellness requirement to reset the 100-day Part A benefit period
CLICK HERE to view the letter on the CMS website
Details of the 3-Day Stay Technical Requirement
As noted in the 2nd paragraph of the above letter, the technical requirement for the 3 midnight hospital stay is temporarily waived for beneficiaries who are affected by the emergency. Of note, this is not a blanket rule to initiate Medicare Part A services for all SNF residents. Specific examples are provided above and justification for each situation should be clearly documented. The Waiver would apply, for example, to residents discharged from the hospital after 1 or 2 nights to the SNF in order to free up the hospital bed for a more seriously ill patient, or those residing in the SNF or from the hospital that need skilled care as a result of the emergency.
Details of the 60-Day Span of Wellness Technical Requirement
As noted in the 3rd paragraph of the above letter, the technical requirement for the 60-day span of wellness to establish one new 100-day benefit period is being waived for a specific set of circumstances. In the document, you will see that the 60-day spell of wellness waiver only applies to those residents currently covered under Part A who just exhausted or may be close to exhausting all 100 days and need to continue Part A due to the emergency circumstances (ie: a delay in discharge from the facility). Of note, the Waiver includes only 1 extra benefit period of up to 100 days based on skilled need.
MDS Submission Requirements
The 1135 Waiver also provides relief to SNFs on the time frame requirements for Minimum Data Set assessments and transmission. This is a blanket waiver for all impacted facilities.
Criteria for Skilled Care & Coverage
With all of the Medicare Part A technical requirement changes, it is important to note that the coverage requirements for skilled nursing and skilled therapy as defined in Chapter 8 of the Medicare Benefit Policy Manual have not changed.
This document will help identify situations that are appropriate for the Medicare Part A Waiver use. 1135 Q&A Document – SNF Page 39
Waiver 1135 Impact on Medicare Part B
The 1135 Waiver made changes to existing rules for Medicare telehealth services effective 3/6/20. Medicare Part B now pays for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence. A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, can offer telehealth to their patients. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
Of note, the Waiver did not change the status of therapists as non-approved telehealth providers. Medicare Part B does not acknowledge physical, occupational and speech therapists as approved telehealth providers. However, the Waiver does allow for the provision of e-visits by therapists.
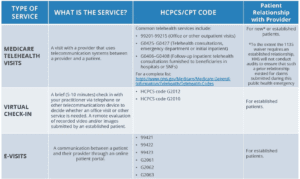
To sort out some of the telehealth confusion, here are three main types of virtual services physicians and other professionals can provide to Medicare beneficiaries under Part B:
• Medicare telehealth visits
• Virtual check-ins
• E-visits (NOT considered as part of Medicare Telehealth)
Each service comes with a unique definition and rule set as defined below. E-visits are currently the only service therapists can bill Medicare Part B for.
The 1135 Waiver has opened up the ability for therapists to provide e-visits {not telehealth} if the requirements for provision are met. Residents under Medicare Part B in the SNF setting are not eligible for reimbursable e-visits since the SNF is the billing provider, not the individual therapist. E-visits are currently limited to therapists in the private practice setting. However, if your SNF is affiliated with an outpatient clinic, and therapists practice under their own provider number, it is possible that e-visits may apply during the 1135 Waiver period. Therapists need to check with their individual Medicare Administrative Contractor (MAC) for details on what is allowable.
This CMS Q&A Document will answer additional questions.
- E-VISITS Defined by CMS
- In all types of locations including the patient’s home, and in all areas (not just rural), established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctor’s office by using online patient portals. These services can only be reported when the billing practice has an established relationship with the patient. For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. The patient must verbally consent to receive virtual check-in services. The Medicare coinsurance and deductible would apply to these services.
- Medicare Part B pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. Practitioners who may independently bill Medicare for evaluation and management visits (for instance, physicians and nurse practitioners) can bill the following codes:
- 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes
- 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes
- 99423: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes.
- Clinicians who may not independently bill for evaluation and management visits (for example – physical therapists, occupational therapists, speech language pathologists, clinical psychologists) can also provide these e-visits and bill the following codes:
- G2061: Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 5–10 minutes
- G2062: Qualified non-physician healthcare professional online assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 11–20 minutes
- G2063: Qualified non-physician qualified healthcare professional assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes.
- E-VISIT KEY TAKEAWAYS:
- These services can only be reported when the billing practice has an established relationship with the patient.
- This is not limited to only rural settings. There are no geographic or location restrictions for these visits.
- Patients communicate with their doctors without going to the doctor’s office by using online patient portals.
- Individual services need to be initiated by the patient; however, practitioners may educate beneficiaries on the availability of the service prior to patient initiation.
- The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G206, as applicable.
- The Medicare coinsurance and deductible would generally apply to these services.
- The use of an online portal, defined as a secure online website that gives patients 24-hour access to personal health information, is described in the original e-visit (pre-pandemic) requirements. However, as you will see below under COVID-19 and HIPAA resources, CMS has relaxed some of the guidelines for technology usage during the pandemic. CMS does not state specific alternate technology for e-visits, though is very specific about telehealth. Before providing e-visits though a non-online-portal-type set up, check with your individual MAC for guidelines to see if the technology platforms listed for approved telehealth can be used for E-visits as well.
Additional Telehealth and E-Visit Resources
Medicare Telehealth FAQ – Released 3/1/7/20
Medicare Telehealth Provider Fact Sheet
CMS Provider Telehealth Toolkit
How To Find Your Medicare Administrative Contractor (MAC)
COVID-19 and HIPAA
The HHS Office for Civil Rights (OCR) announced on March 17, 2020, that it will waive potential HIPAA penalties for good faith use of telehealth during the nationwide public health emergency due to COVID-19. The notifications below explain how covered health care providers can use everyday communications technologies to offer telehealth to patients responsibly.
- Notice of Enforcement Discretion for Telehealth
- Under this Notice, covered health care providers may use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype, to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules related to the good faith provision of telehealth during the COVID-19 nationwide public health emergency.
- FAQs on HIPAA and Telehealth – PDF
- A “non-public facing” remote communication product is one that, as a default, allows only the intended parties to participate in the communication. Non-public facing remote communication products would include, for example, platforms such as Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Whatsapp video chat, or Skype. Such products also would include commonly used texting applications such as Signal, Jabber, Facebook Messenger, Google Hangouts, Whatsapp, or iMessage
- March 2020 HIPAA and COVID-19 Bulletin – PDF
- FAQ Telehealth and HIPAA
APTA, AOTA and ASHA are currently advocating for changes to allow therapists to provide telehealth. Keep an eye on your professional associations as they can direct you as to how to assist in the advocacy efforts. Also, some private insurers and Medicare Advantage plans throughout the country have temporarily allowed therapists to participate in and bill for telehealth as well.
Other Important Links
- Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes- Issued 3/13/20
- Includes directives for visitors, group activities/therapy
- AHCA-NCAL Statement: The Role of Physical and Occupational Therapy and Speech-Language Pathology Personnel in LTC Facilities During the COVID-19 Pandemic
- CDC Home Page for COVID-19 Statistics By State
- State Practice Act Links for PT, OT and Speech
Potential For Additional Changes
Again, the regulatory environment is currently very fluid and we can expect additional changes. APTA, AOTA and ASHA are heavily advocating for change in the telehealth regulation to recognize therapists as approved providers, so that therapists can begin providing reimbursable Part B services to seniors, both during the current pandemic and into the future.
If you have any questions about any of the above information or need additional information, use our Just Ask Q&A Forum and one of our team members will respond to you directly to assist.
For all you do to protect the greatest generation, thank you.
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
The Montero Therapy Team
SNF Rehab and MDS Compliance Experts
www.MonteroTherapyServices.com

Awesome stuff you guys. Thank you for the summary
Thanks, Bob! Stay safe out there!