 CMS was busy, busy, busy this past week….
CMS was busy, busy, busy this past week….
CMS released the Medicare Part A Skilled Nursing Facility Prospective Payment System (SNF PPS) FY2020 Final Rule taking effect 10/1/19. [Click to access the 364 page Rule]
and
the Medicare Part B Physician Fee Schedule(PFS) Proposed Rule, previewing what will kick in 1/1/20, unless changes are made in the Final Rule due to be released in the fall. [Click to access the 1704 page Rule]
Let’s take a quick look at the highlights from each rule that are most pertinent to therapy professionals in the SNF setting.
SNF PPS Final Rule: Medicare Part A Changes
The SNF PPS Final Rule addresses changes to 3 main components of Medicare Part A:
- SNF PPS payment policy under the SNF Prospective Payment System [PDPM info]
- SNF Value-Based Purchasing Program (VBP)
- SNF Quality Reporting Program (QRP) [MDS Section GG info]
If you need to brush up on the specifics of each of these programs, this article will catch you up to speed. Here are the highlights from the Rule for each:
1- SNF PPS
Yes….PDPM is still set to begin 10/1/19. In addition to everything we anticipated, the Final Rule provided 2 key additional pieces of information:
- PDPM Component Rates
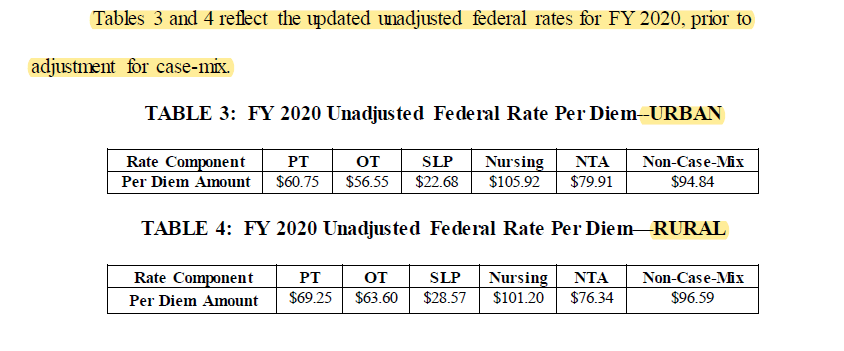
The Federal Per Diem rates are updated every year with each Final Rule. We can now replace the rates we were using from the prior Rule with these new rates set for 10/1/19. These are the rates that then need to be adjusted based on the Case Mix Index the resident falls into for each of the 5 PDPM Components.
- Revised Group Therapy Definition
As was alluded to in the Proposed Rule a few months ago, CMS noted the definition for Part A Group Therapy in the SNF may be adjusted. This did indeed happen and effective October 1, 2019, Group Therapy will be defined as “a qualified rehabilitation therapist or therapy assistant treating two to six patients at the same time who are performing the same or similar activities.”
CMS reiterated on multiple pages in the Final Rule, as they did in the Proposed Rule, that only the clinician can determine if group therapy is appropriate, as well as determining the appropriate type and size of the group. CMS also restated that individual therapy is the preferred mode and if group [or concurrent] is used, there must be documentation to justify the medical necessity of these modes.
- The PPS 5-Day MDS
The PPS 5-day MDS assessment, typically called the “5-day”, will now be referred to as the “Initial Medicare Assessment.” Because PDPM eliminated the bulk of scheduled MDS PPS assessments [A.K.A the 14-day, 30-day, 60-day and 90-day], the 5-day MDS name was changed to better reflect what it is under PDPM, the Initial Medicare Assessment.
2- SNF Value-Based Purchasing Program (SNF VBP)
The SNF VBP Program has been with us for over a year and is part of the shift CMS is taking toward paying based on quality rather than quantity – or “value over volume.” The program reduces SNF Medicare payments to all SNFs by 2% and then allows for an opportunity to recoup all or part of the 2% by demonstrating success with the established Quality Measure. The current measure in this program is the SNF 30-Day-All-Cause Readmission Measure (SNFRM – NQF #2510). In essence, this measures if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital.
There are no significant changes that impact SNF therapy at this time. Please refer to this article to obtain specifics on the SNF VBP, including information SNF therapy professionals need to know.
3- SNF Quality Reporting Program (SNF QRP)
The SNF QRP is the program behind Section GG, as well as other MDS data collection to measure multiple areas of care. See below for the current measures in place.
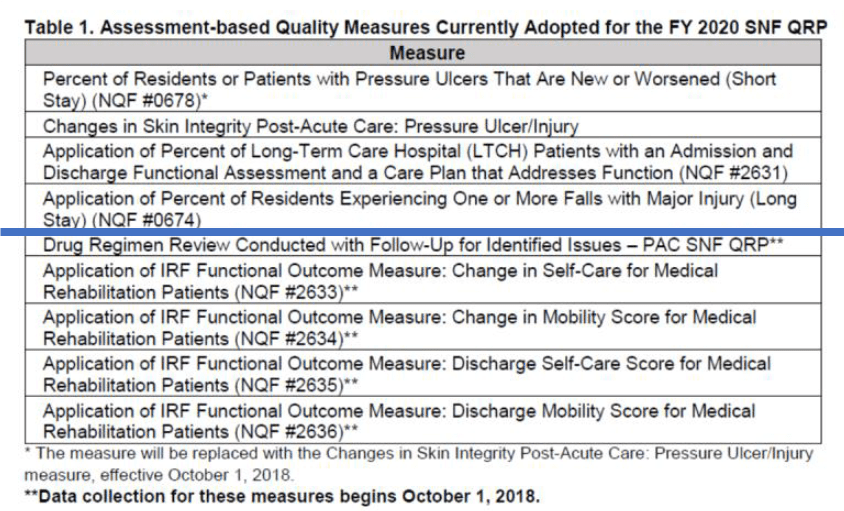
CMS is adopting two new quality measures in FY 2020 to assess whether certain health information is provided by the SNF at the time of transfer or discharge. The two measures are: 1) Transfer of Health Information to the Provider-Post-Acute Care and 2) Transfer of Health Information to the Patient-Post-Acute Care.
CMS is also adopting new standardized patient assessment data elements, each of which assesses one of the following categories: cognitive function and mental status, special services, treatments and interventions, medical conditions and comorbidities, impairments, or social determinants of health.
Together, the Transfer of Health Information measures and the standardized patient assessment data elements would require SNFs to begin reporting on or after October 1, 2020.
SNF Physician Fee Schedule (PFS) Proposed Rule: Medicare Part B Changes
The Proposed Rule is only 1704 pages… and though we will need to wait for the Final Rule in October, we can project that the following changes will take place January 1st:
Reduction of Payment for Part B Services Provided by Assistants (PTA, COTA/OTA)
- All therapy services on or after 1/1/2020 provided in whole or in part by an Assistant will need to be billed using the new payment modifiers. This will allow CMS 2 years of data collection to assess potential revisions to the requirements before the payment reduction kicks in 1/1/22. Here are the new modifiers:
- New PTA Payment Modifier: CQ
- New OTA Payment Modifier: CO
- All therapy services on or after 1/1/2022 provided in whole or in part by an Assistant will have a payment reduction of 15% applied
What does “provided in whole or in part” mean?
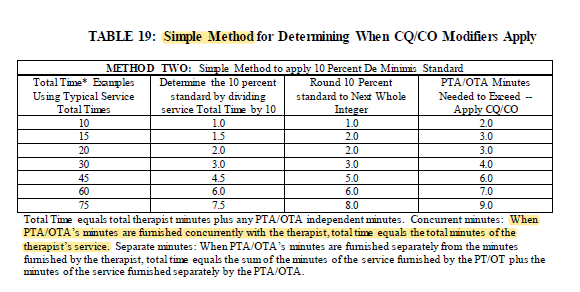
CMS is defining in whole or in part as provision of more than 10% of a therapy service by an assistant. This “more than 10%” is considered a de minimis standard.
What does “therapy service” mean?
A therapy service is a “procedure” identified by a HCPCS code {A.K.A. CPT Code} . On a Part B claim, each “procedure” is identified line by line to include CPT codes, units and modifiers. The new modifiers would be added specifically to the procedure line item to show an assistant provided treatment that met the de minimis standard.
The Proposed Rule contains multiple examples of when the new modifiers would be needed….and if an assistant is participating in even a minimal portion of a treatment either with or without the therapist, the modifiers would likely be indicated on a portion of the procedure codes. A surprising example was the need for the modifier when the assistant is treating with the therapist, and the time spent by the assistant is greater than 10% of the total treatment. For example, if a resident had a 30 minute treatment by the therapist, and the assistant participated in 4 or more minutes of the session with the therapist, the modifier would be needed.
This chart was included to assist with determining when to apply the modifiers.
The Proposed Rule also identifies the need for therapy documentation to be able to identify the total treatment time and the exact time an assistant provided treatment. The Rule referenced using daily treatment notes to include this information.
Here is an excerpt from the Rule regarding documentation changes:
“We propose to add a requirement that the treatment notes explain, via a short phrase or statement, the application or non-application of the CQ/CO modifier for each service furnished that day. Because the CQ/CO modifiers also apply to untimed services, our proposal to revise our documentation requirement for the daily treatment note extends to those codes and services as well. For example, when PTAs/OTAs assist PTs/OTs to furnish services, the treatment note could state one of the following, as applicable: (a) “Code 97110: CQ/CO modifier applied ‒ PTA/OTA wholly furnished”; or, (b) “Code 97150: CQ/CO modifier applied ‒ PTA/OTA minutes = 15%”; or “Code 97530: CQ/CP modifier not applied ‒ PTA/OTA minutes less than 10% standard.” For those therapy services furnished exclusively by therapists without the use of PTAs/OTA, the PT/OT could note one of the following: “CQ/CO modifier NA”, or “CQ/CO modifier NA ‒ PT/OT fully furnished all services.”
In Summary
Change in the SNF is what we are used to. Every year. Without fail.
10/1/19 and 1/1/20 will introduce significant changes for both the Medicare Part A and Medicare Part B payment models, as well as all therapy software programs and facility EMR’s, but it is nothing that we as SNF therapy professionals can’t handle!
Keep an eye out for in depth articles for both the Part A and Part B changes. Once we fully dissect both Rules, we will have additional information for you!
In the meantime, if you have any questions, send them to our Just Ask Q&A Forum. You can also take a peek at all the other questions your peers are asking.
In Your Corner,
Dolores and the Montero Therapy Team
SNF Therapy & MDS Compliance Experts

The proposed reimbursement cut for assistances is going to be harmful to our patients. Instead of receiving quality rehabilitative services, there will be many cases of untreated patients due to lack of evaluating therapist.