Think back to the fall of 2014…Does the IMPACT Act ring any bells?
Think back to the fall of 2014…Does the IMPACT Act ring any bells?
Maybe it sparked your interest at the time and then faded into the backgroud with all the other changes in LTC. Well, SNF’s will soon feel the IMPACT of this Act…so NOW is the time to get caught up…before it’s too late.
A Little History
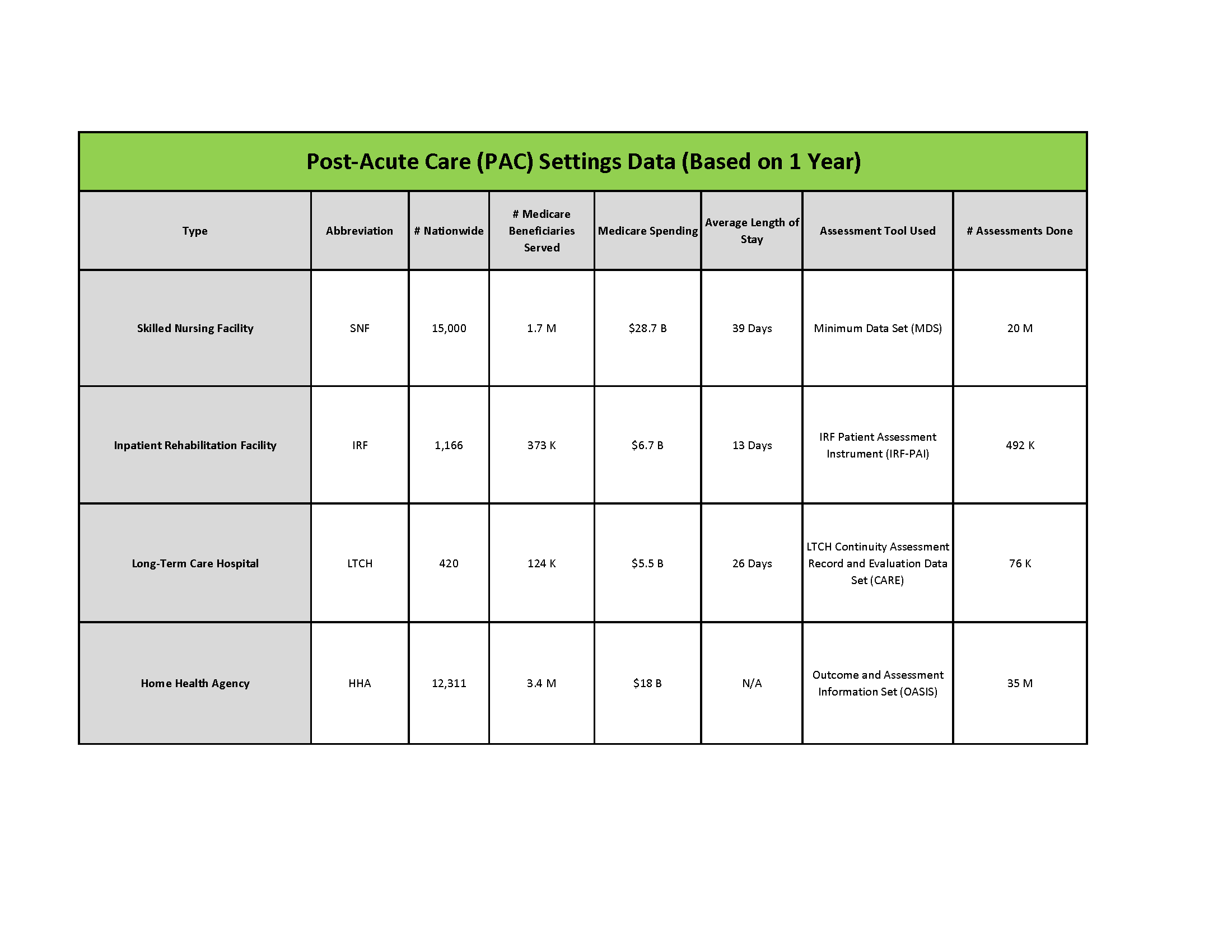
On September 18, 2014, Congress passed the Improving Medicare Post-Acute Care Transformation Act of 2014 (the IMPACT Act). The Act requires the submission of standardized data by Long-Term Care Hospitals (LTCHs), Skilled Nursing Facilities (SNFs), Home Health Agencies (HHAs) and Inpatient Rehabilitation Facilities (IRFs). The IMPACT Act established a quality reporting program (QRP) for SNFs. (This is different from QM 5 Star NH Compare program.)
This was the Act that was going to potentially change our assessment process in post-acute care settings (PAC). Remember “GG?”
The IMPACT Act of 2014 required the following:
- Secretary to implement specified clinical assessment domains using standardized (uniform) data elements to be nested within the assessment instruments currently required for submission by LTCH, IRF, SNF, and HHA providers.
- CMS develop and implement quality measures from five quality measure domains using standardized assessment data.
- Development and reporting of measures pertaining to resource use, hospitalization, and discharge to the community.
The intent of the Act was to make a step towards value based payment, where rates could be established based on patient characteristics by:
- Unifying data elements and comparison across settings
- Improving quality of care and outcomes through improved information sharing
- Improving discharge planning by supporting transitions
- Coordinating care
A Few PAC Setting (Post-Acute Care) Facts:
Through the use of standardized quality measures and standardized data, the Act serves to achieve a “triple aim” of:
- Better Care: Improve the overall quality of care by making healthcare more patient-centered, reliable, accessible, and safe.
- Healthy People, Healthy Communities: Improve the health of the U.S. population by supporting proven interventions to address behavioral, social, and environmental determinants of health in addition to delivering higher-quality care.
- Affordable Care: Reduce the cost of quality healthcare for individuals, families, employers, and government.
What SNF Professionals Need to Know Now
When Does This Start: Data collection starts October 1, 2016 and the first phase lasts for 3 months through December 31, 2016
Who Is Involved: Data collection is for traditional Medicare Part A residents only
What Is Being Collected: New data for residents that are admitted and discharged from Medicare Part A. This includes residents that are discharged from the facility (planned), as well as those that stay long term
What Is the New Data:
To put it simply….Falls…Skin…and Function. Well…there’s more but we will save that for another day. For now, let’s focus on the MDS based changes.
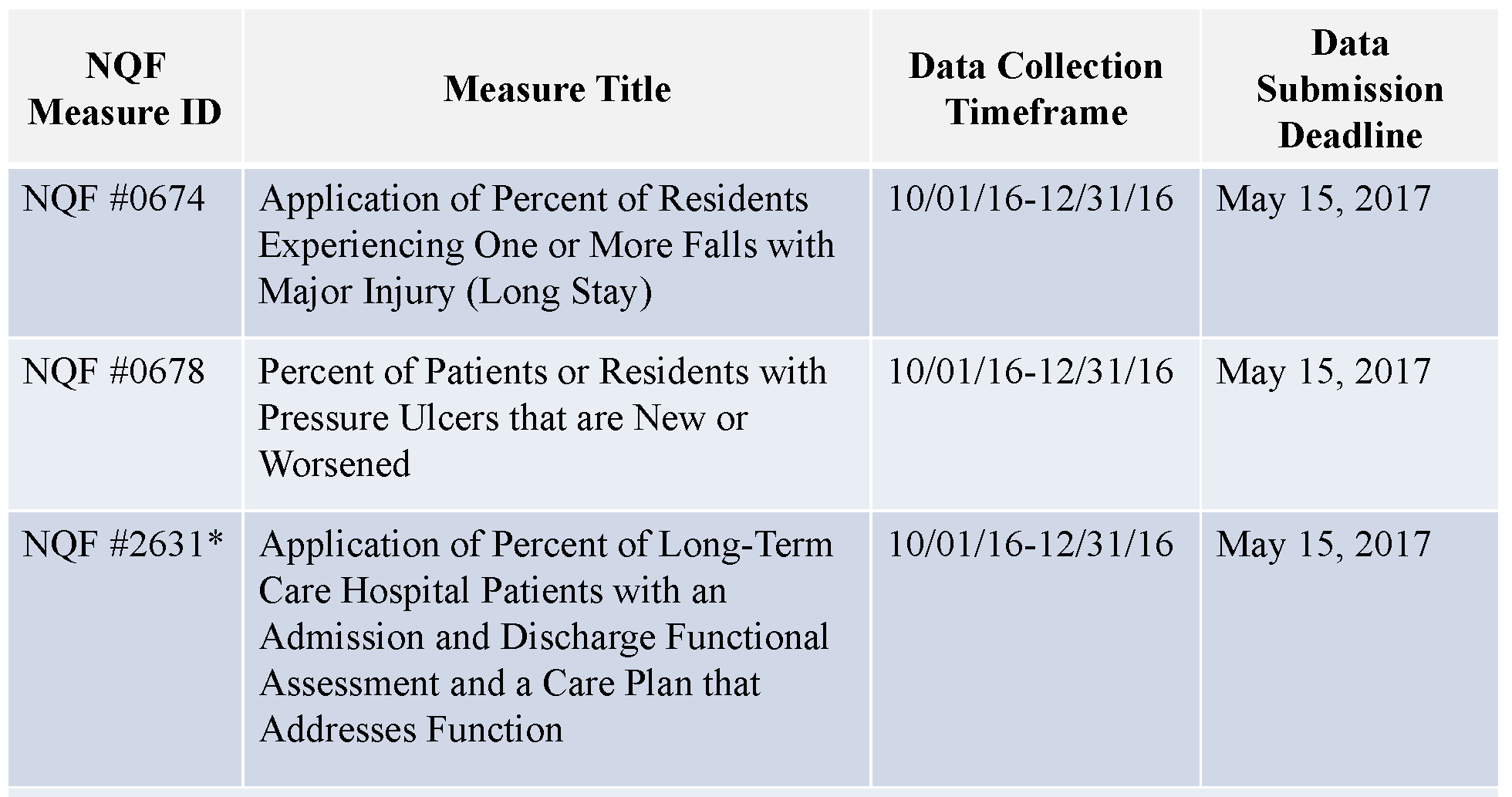
Remember, this is not your 5 Star rating. Some of the above categories already exists in the form of a Quality Measure for 5 Star NH Compare (like Falls and Skin), but the calculation for this QRP will be different.
How Will This Data Be Collected: In the SNF setting, the MDS will collect the data. For Skin and Falls, MDS questions are already present that will be used.
- Falls with Major Injury: MDS Question J1900C
- Skin: MDS Question M0800/M1313
For the new data, Function, there is now a new section called “GG.” In this section, Function is broken down into Self Care and Mobility. Some of the items may sound familiar as they are currently in Section G – though these new items in “GG” will be scored using a totally different scale.
Self Care, New Section GG0130, includes:
- Eating
- Oral Hygiene
- Toileting Hygiene
Mobility, New Section GG0170, includes:
- Rolling
- Supine-Sit
- Transfer Bed-Chair
- Toilet Transfer
- Walk 50′ with 2 turns
- Walk 150′
- Wheel 50′ with 2 turns
- Wheel 150′
Want To See Section GG For Yourself? Click for PPS MDS | Click for Discharge Med A MDS
What Type of MDS Will Collect the Data: Since the data is required for all residents admitted and discharged from Medicare Part A, the PPS 5-Day will be used for admissions to Part A, and a Discharge MDS will be used for discontinuation of Part A. Modifications have been made to each type of MDS to allow for the appropriate data collection.
Who Fills Out Section GG: Well, the RAI Manual is not updated yet, but it is anticipated that this will be left up to each SNF. The assessments will have a specified time frame in which the data is required. Admission data will be required by day 3 – which will likely change existing SNF facility policy. Some Rehab software companies have added the additional “GG” questions to their data collection in an attempt to prepare for any changes.
What Happens If Data Is Missing: If SNF’s do not supply data during the 3 month collection period, they will suffer a payment penalty. A 2% reduction to the Part A Revenue for the Entire FY 2018 market basket percentage will occur….based on what happens from October to December. The penalty is for missing data – NOT outcomes. Missing data includes blanks or dashes in the assessment questions. Then the data collection timeline will progress into FY 2017 which will impact FY 2019, etc.
What Do SNF’s Do Next: It is time to look into your current operational policy for the MDS and determine who should take the lead on ensuring these new sections are completed correctly prior to the October 1st implementation date. Administration, nursing and therapy need to collaborate on how these new tasks will be accomplished. SNF’s need to look at the following:
- Where will the information to fill out Section GG come from? If therapy is deemed responsible, how will the information be provided if the resident is not on therapy for the Part A stay in question?
- Who will provide education in your facility as to the specific requirements for the data collection, including rule for MDS coding?
- Who will sign MDS Section GG?
- Await the updates in the Proposed/Final Rule to ensure your staff have specific information needed
Change…
CMS is on a roll….More changes are coming to the QRP and to Quality Measures. As we eagerly await the 2017 Proposed Rule, we can only imagine what’s next!
Stay tuned for more updates and explanations on Section GG and changes to come that will impact SNF therapy.
As always, any questions can be submitted to our Just Ask! Q&Q Forum.
In Your Corner,
Dolores
www.MonteroTherapyServices.com