Have “G-Codes” made their way into the SNF MDS ? Read on and see what you think!
? Read on and see what you think!
The new collection of “function-based” data for SNF residents in a Medicare Part A stay will begin this October 1st and some therapists may experience a déjà vu. Functional abilities, self-care, mobility, current status, goal status and discharge status...sound familiar? If you are familiar with Medicare Part B therapy, it sure does!
So what is happening in the SNF setting October 1st?
The upcoming changes reach far beyond SNF therapy and stem from Medicare’s desire to transform care coordination, resource use and outcomes across Post-Acute Care (PAC) settings. For a detailed explanation of the When’s, Why’s and How’s of the upcoming changes, read our earlier article by clicking here. This info will get you caught up to speed on the Impact Act, Quality Reporting Program and the goal of standardized assessment data between PAC settings, including Home Health, Inpatient Rehab, Long Term Care Hospitals and Skilled Nursing Facilities.
Now let’s move ahead to what the changes will be and how they will impact the SNF therapist.
What Will Be New?
The MDS 3.0 will add new questions about functional status in the areas of Self-Care and Mobility. The data collected will be contained in a new section, “Section GG: Functional Abilities and Goals,” and will be required at the beginning and end of Medicare Part A stays that meet certain criteria. The current MDS Section G: ADL’s, will not change. Section G has historically been completed from nursing documentation, where the new Section GG will require input from Therapy, and may even take information directly from therapy documentation.
The new question areas are as follows:
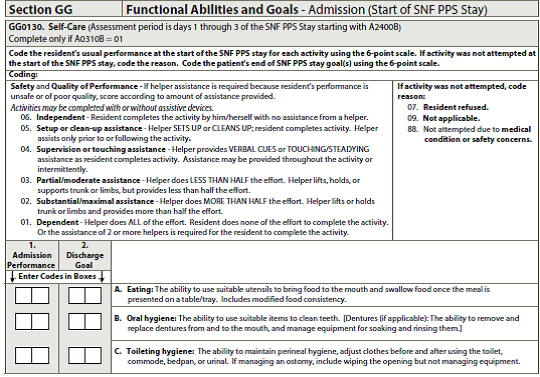
Self-Care, New Section GG0130:
- Eating: ability to bring food to mouth once presented on a tray
- Oral Hygiene: ability to clean teeth and/or dentures
- Toileting Hygiene: ability to maintain perineal hygiene, adjust clothes pre/post toilet, commode, bedpan
Mobility, New Section GG0170:
- Sit to lying: sitting on edge of bed to lying flat
- Lying to sitting on edge of bed: feet flat on floor, no back support
- Sit to stand
- Chair/bed-to chair transfer
- Toilet transfer: on and off toilet or commode
- Does the resident walk? Answer if walking will be a goal or not
- Walk 50′ with 2 turns
- Walk 150′
- Does resident use a wheelchair or scooter?
- Wheel 50′ with 2 turns
- Wheel 150′
Take a look at what the actual MDS draft version looks like below.
Self-Care
Mobility
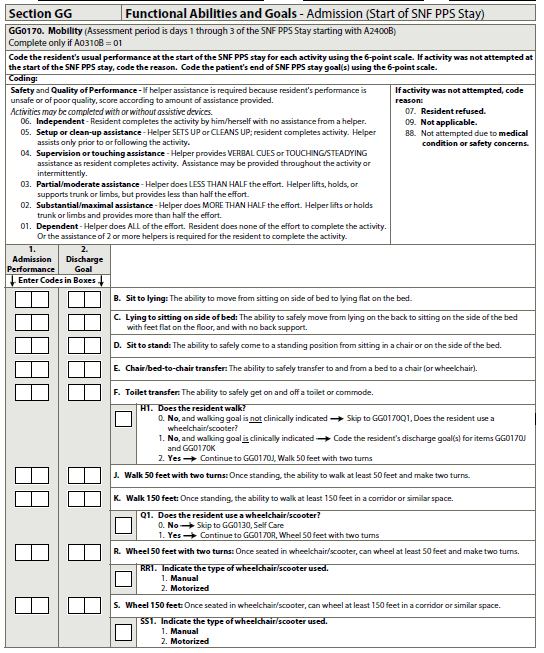
How Are the Answers Coded?
Section GG uses a 6 point scale ranging in levels of assistance provided by a “helper,” or in other words, what did the “helper” do? Coding should reflect “usual performance in the look-back period,” so these questions can’t be answered by a one-shot screen or evaluation; coding needs to reflect the “usual status” by blending together data from multiple sources.
The scores are as follows…oh, and finally some MDS language that therapy can relate to!
- 01 = Dependent
- 02 = Substantial/Maximal Assist
- 03 = Partial/Moderate Assist
- 04= Supervision or Touching Assist
- 05 = Setup or clean-up assist
- 06 = Independent
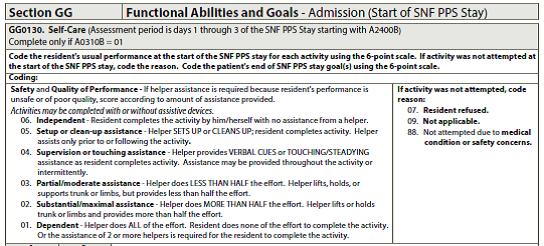
There are some other optional answers for instances when the functional activity was intentionally not attempted. Why these codes are very important is discussed later.
- 07 = Resident refused
- 08 = Not applicable (ie: Toilet transfer for a resident who is a bed check and change would be 08)
- 88 = Not attempted due to medical or safety concern
Who Is Section GG Data Collection For?
- Traditional Medicare Part A residents only. This excludes Managed Medicare or any insurance that pays your facility by RUG score. {If you are doing PPS assessments on non-Medicare Part A residents for billing purposes, you will need to sort through some potential issues and pitfalls.}
- Residents who are discharged from Medicare Part A and either leave the SNF or stay long-term, as long as the discharge was “planned.” How is “planned” determined? Question A0310G on the MDS flat out asks “Type of Discharge: Planned or Unplanned.” If “planned” is selected, Section GG will be required on the DC MDS. Planned could include discharges to the community, the same or another SNF, to an IRF, Hospice, etc.
- Residents with a Medicare Part A stay of at least 3 paid days.
Where Will Section GG Show Up and What Is the Look-back Period?
Since data collection is required for all residents Admitted and Discharged from a Medicare Part A stay, the current PPS 5-Day MDS will be used for Admissions to Part A, and a new Discharge MDS was created and will be used for the Discontinuation of Part A stay.
- 5-Day PPS MDS: Section GG will appear on the existing 5-Day MDS. The Self-Care and Mobility questions will require coding for the “Admission Performance,” which is defined as the “usual performance on PPS Day 1, Day 2 and Day 3” of the Medicare Part A stay only – so the look-back for these questions will always be the 1st 3 days of the stay – whether therapy is involved or not.
- On the 5-Day PPS MDS, Section GG will also include an additional component… and here is where that déjà vu comes in. Not only is the “Admission Performance” coded using the 0-6 point scale, GG will also require the SNF to project the resident’s status on Discharge from the Medicare Part A stay by coding “Discharge Goals” for each Self-Care and Mobility area. In other words, on admission, function is completed for the resident’s current status and projected status at discharge for each of the functional items. {Sound like Functional Limitation Reporting / G-Codes yet?}.
- Discharge End of PPS Stay MDS: Section GG on the new Discharge “End of SNF PPS Stay” assessment includes coding for the discharge performance status in each area. The data collection / look-back period for Section GG for the discharge is fixed as the last 3 paid PPS days.
- Section GG has a fixed 3 day look back period vs the traditional 7 day look back AND the lookback is not dependent on an ARD. The lookback periods are determined by the 1st and last covered Medicare Part A day.
What Happens If Data Is Missing?
If SNF’s do not supply data during the 3 month collection period {Oct 1-Dec 31 2016}, they will suffer a payment penalty. A 2% reduction to the Part A Revenue for the Entire FY 2018 market basket percentage will occur….based on what happens from October to December. The penalty is for missing data – NOT poor outcomes. Section GG outcome performance is not currently tied to reimbursement like Section G is {remember, Section G determines the ADL score}. Currently the focus is data collection.
Dashes in Section GG is equivalent to Missing Data
Ensure coding of GG does not include dashes
Remember, Section GG is tied to the Quality {Measure} Reporting Program and all data collected will fall under the measure of “% of residents with and admission and discharge functional assessment and a care plan that addresses function.” At some point outcomes will drive payment…just not yet. {Just like Medicare Part B – FLR}
In a Nutshell
- SNF Traditional Medicare Part A residents will require completion of Section GG when a Part A stay begins and ends, using a specific item set and a fixed 3 day lookback period.
- Therapy will be heavily relied upon to provide admission and discharge status data for the Self-Care and Mobility areas, as well as help predict the resident’s functional discharge status at the time of admission {goal setting has never been a part of the MDS before and the Clinical Team may need your help!}
- Therapy data for these questions will need to be used in combination with nursing data since the 3 day lookback period includes the resident’s “usual performance” and not the snapshot performance that a therapy evaluation and/or discharge summary would provide
- Coding of Section GG should be completed by Nursing – not Therapy – though a team discussion is a must, with review of all clinical documentation
So, after October 1st, Medicare will begin acquiring data on Self-Care and Mobility at the start and end of Medicare Part A, which is often the start and end of therapy. Medicare will be able to see if progress was predicted AND if progress was achieved. What do you think this this data will be used for? Hmmm…say the discharge MDS does not show progress in function, yet the resident received Ultra High therapy for 60 days, for example… Something to think about…
As far as the MDS changes and new questions, SNF therapists this is what you do every day in your therapy plan of care….Evaluate…Set Goals…Predict Discharge Outcomes…Assess at Discharge…
SNF therapists, you’ve got this! …Lather…Rinse…Repeat!
Any questions on this topic, visit our Just Ask! Q&A Forum! OR
Join Us on Thursday, September 1st 12:00pm to 1:15 pm EST for a live webinar “MDS Section GG: Guide for SNF Therapists,” to review therapy- specific information, recommendations for practice and live Q&A!
“MDS Section GG: Guide for SNF Therapists,” to review therapy- specific information, recommendations for practice and live Q&A!
In Your Corner,
Dolores
Free Resources for more info on this topic:
The Impact Act – Info for Therapists
SNF Quality Reporting Program Measures Explained
Draft RAI Manual with Section GG Information May 2016 (Final Manual due late summer)
Want To See Section GG For Yourself? Click for PPS MDS | Click for Discharge Med A MDS
Want more info?
Check out this COURSE
