CMS released the “Medicare Part B” Physician Fee Schedule (PFS) FINAL RULE last week outlining what will kick in 1/1/21. [Click to access Rule]
This 2,165 page final rule included tying together information from the March 31st, May 8th and September 2, 2020 Rules released in response to the Public Health Emergency (PHE) for the Coronavirus Disease 2019 (COVID-19). This Final Rule also contains an Interim Final Rule to establish coding and payment for virtual check-in audio-only services.
There are definitely a lot of rules floating around out there…some temporary due to the PHE, and some permanent. We sorted them out and highlighted the ones that are most pertinent to SNF therapy professionals. Let’s go!
What Do SNF Therapists Need to Know for January 1st, 2021?
1. Rate Information
Therapy Cap
-
- The cap is gone and is not coming back! But…..the Therapy Cap is now disguised as the KX Modifier Threshold
- Continued use of the KX modifier is required for all therapy services that “would have exceeded the previous therapy cap amounts”
- Therapy services over the “threshold” without the KX modifier will be denied
- New “threshold” for 2021 is $2110 for OT, $2110 for PT and Speech combined (up from this year’s amount of $2080)
- Important reminder of what the KX Modifier means:
- “By applying the KX modifier to the claim, the therapist or therapy provider is confirming that the services are medically necessary as justified by appropriate documentation in the medical record.”
Manual Medical Review
-
- The manual medical review threshold continues at the same amount of $3000 until 2028
- Review is not automatic when the $3000 is reached. CMS is using targeted reviews, limiting reviews to “outliers” and those with questionable practice patterns
The Conversion Factor (CF)
-
- The CF for 2021 is $32.41, down from $36.09 in 2020
- What does this mean? The CF is part of a formula that converts Relative Value Units (RVU) to dollar amounts. If the CF is down, the overall payment rate for the CPT codes will be down, unless the RVU value for a particular CPT code goes up
- For the math geeks: Payment = [(RVU work x GPCI work) + (RVU PE x GPCI PE) + (RVU MP x GPCIMP)] x CF
Cuts Averaging 9% for PT/OT and Speech/Audiology Services
-
- Not all PT, OT and Speech services will be cut by 9%. It will depend on the CPT code, as noted above in the CF calculation.
- The extent that the cuts will impact your facility depends on your practice patterns and codes you typically bill
- Why the cuts?
- To balance the adjustments made to Evaluation and Management (E/M) codes used by other specialties, primarily physicians.
- In order to keep a balanced budget, if the value of some CPT codes go up, the value of others must come down. In this case, the value of E/M codes used by physicians will increase, resulting in a decrease in the value of some “therapy codes,” as well as codes used by other specialties
- And CMS also reminded us of the 15% payment reduction for services [CPT codes] provided in whole or in part by PTA’s and C/OTA’s coming in 2022. If you need to brush up on that information, this article is very helpful.
Any Good News?
-
- Yes! The therapy evaluation and re-evaluation codes have been “re-valued” and will see a significant increase (average of 28% increase in the work RVU in the formula above thus increasing reimbursement for these codes).
- Codes impacted include these found on page 254:
- PT Eval/Re-Eval: 97161, 97162, 97163; 97164
- OT Eval/Re-Eval: 97165, 97166, 97167, 97168
- SLP Communication Evaluations: 92521, 92522, 92523, 92524 […of note, the Swallowing Eval code is not included]
- Did you know you can look up any CPT code and check the rate HERE ?
2. Virtual Services and Telehealth
-
- Virtual Services is the umbrella category where Telehealth lives. Telehealth is a Virtual Service but all Virtual Services are not considered Telehealth. This is an important distinction to understand when looking at the rules. This article may help clear up any confusion.
- Virtual Services encompasses Telehealth, E-Visits, Virtual Check-Ins and Telephone E/M services.
- In the Final Rule, CMS reiterates that Telehealth is defined as remotely providing the services when not in the same location as the patient (off-site vs in another room), and if in the same location as the patient, the services are not considered telehealth
- Therapists were not able to provide telehealth services prior to the Public Health Emergency (PHE)
- Therapists are only able to provide telehealth now through waiver authority under section 1135(b)(8) of the Act, in response to the PHE for COVID–19. Why? Because CMS removed the geographic and site of service originating site restrictions in section 1834(m)(4)(C) of the Act, as well as the restrictions in section 1834(m)(4)(E) of the Act on the types of practitioners who may furnish telehealth services, for the duration of the PHE for COVID–19
- At the conclusion of the PHE for COVID–19, these waivers and interim policies will expire, payment for Medicare telehealth services will once again be limited by the requirements of section 1834(m) of the Act
- What does this mean for therapists:
- When the PHE ends, all temporary rules, including allowing therapy professionals to provide telehealth, will end
- When the PHE ends, there will be some “therapy” codes that remain in effect through the calendar year end….but even though these codes stay alive, therapists will not be able to provide and bill Medicare for these services, as our temporary permissions will have expired (don’t forget that others professionals can bill these codes)
- On a positive note, a limited number of therapy codes were added to a new CMS category, “Category 3,” which is a temporary category where the codes will live until the end of the year that the PHE ends, and will allow for continued discussion about future potential use. No “therapy” codes were in the Proposed Rule, so this, at least, is progress.
- Any service added under the proposed Category 3 would remain on the Medicare telehealth services list through the calendar year in which the PHE for COVID–19 ends (but this does not mean therapists will be able to provide and bill…)
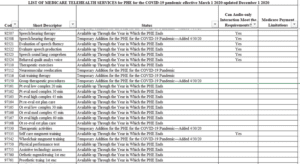
- What’s missing from the list? The 4 codes that were most recently added during the PHE: 97530, 97542, 97150 and 92508. These 4 will end with the PHE. See Table 16

-
- Below is the updated list of CPT codes for telehealth for therapy professionals to use for the PHE duration:
-
- Other Virtual Services (Non-telehealth)
- Virtual Check-In’s will remain for therapists after the PHE, with the addition of new codes G2250, G2251 for therapists in private practice
- E-Visits will remain for therapists after the PHE, though for private practice only. G2061, G2062, G2063 transitioning to 98970, 98971, 98972 (though further clarification from CMS is needed on this)
- Telephone E/M Services for therapists will not continue after the PHE, which eliminates codes 98966, 98967, 98968
- Other Virtual Services (Non-telehealth)
3. Direct Supervision by Interactive Telecommunications Technology
-
- The Final Rule extends the PHE rule for providing direct supervision via audio visual technology through 12/31/2021
- This does not impact the SNF setting specifically as Medicare Part A and Part B in the SNF currently require “general supervision,” meaning a therapist does not need to be in the room or on site in order for an assistant to provide services. Medicare Part B supervision rules for Private Practice, however, are more strict. This rules is geared more toward physicians and medical practitioners
- Do not confuse this rule with your State Practice Act requirements for supervision. This is only a Medicare payment regulation based on Medicare’s definition of Direct Supervision, and State Practice Acts may require on-site supervision, pandemic or not.
4. Provision of Maintenance Therapy PTA’s and C/OTA’s
-
- The Rule finalizes changes to the Medicare Benefit Policy Manual Chapter 15 requirement for skilled maintenance therapy which currently states skilled maintenance therapy must be provided by a therapist in a Part B setting. The new rule will allow the PTA and C/OTA to provide maintenance therapy, if delegated and supervised by the therapist
- This is currently a temporary rule under the PHE for 2020 and will become permanent 1/1/21
5. Documentation
-
- The Final Rule states a clarification to the existing rule from last year regarding therapy student documentation, and the ability for a therapist to “review and verify” documentation in the medical record, rather than re-document everything the student noted. CMS defines “review and verify” as “sign and date,” and directly applies it to the clinician that is billing Medicare for the documented services.
- This Rule does not have anything to do with the delegation of documentation a therapist is required to complete by Medicare regulation (ie: progress report, evaluation, re-evaluation, plan of care, etc) to a therapist/therapy assistant.
6. Important Links and Resources
- CMS Physician Fee Schedule Home Page
- CMS List of Covered Telehealth Services Updated 12/2/20
- All Downloads for PFS Final Rule CY2021
- FAQ for Part B Billing – COVID-19 Changes
- CMS PHE COVID-19 Medicare Document – Rule Changes
Change Happens
After enduring almost 1 year of a pandemic, these changes seem pretty minor, and SNF therapy professionals can handle them!
Remember, these changes are for Part B therapy only, and specific to the SNF setting. We teased out the parts of the Rule that applied to the SNF….and don’t need to worry about MIPS or other rules specific to private practice [thankfully!]
As always, if you have any questions about the information or how it will impact you, send them to our Just Ask Q&A Forum. There you can also take a peek at all the other questions your peers are asking.
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Rehab and MDS Compliance Team