CMS released the Physician Fee Schedule (PFS) Proposed Rule, or the “Medicare Part B Rules,” outlining what kicks in 1/1/23, unless changes are made prior to the release of the Final Rule later this fall.
This 2,066- page document includes information on payment rate changes, new codes, supervision of assistants, telehealth and more! We highlighted the Medicare Part B rules that are most pertinent to therapy in the SNF setting.
So let’s take a look….
Proposed Changes for January 1st, 2023?
1. Rate Information
Rate cuts have been a constant for the last few years, and 2023 will be no different. CMS is proposing a 4.4% decrease from CY2022.
For the last 2 years, larger cuts were expected for therapy services due to the re-valuation of multiple Current Procedural Terminology (CPT) Codes. The codes used by physicians {Evaluation and Management Codes} increased in value, therefore, in order to maintain a neutral budget, other CPT codes needed to be reduced, including those used by PT, OT and Speech. The only reason we did not see the staggering cuts {9%} that were planned for the last 2 years was because Congress intervened at the last minute, providing additional funds to offset the cuts.
The 4.4% cuts for CY2023 are in part due to the expiration of the 3% “intervention” from Congress last year ending 12/31/22, and an additional 1.4% cut to neutral-out the values of the codes as noted above.
So here we are again, year 3, waiting to see if the proposed cuts will take place as is, or if there will be an intervention to soften the blow. 4.4% is what we can expect at the moment.
Cuts explained….
Cuts can be attributed to a decrease in the Conversion Factor (CF). This is a value that CMS modifies yearly, and is part of the formula that determines the dollar amount for each CPT code by converting Relative Value Units (RVU). The CF impacts all CPT Codes across the board. When the CF decreases, the overall payment rate for the CPT codes decrease, unless the RVU for a specific CPT code is increased enough to offset the CF drop.
The CF has not been trending in a favorable way over the past 4 years, hitting a 20-year low for 2023. The CF for 2023 is $33.08, dropping from $34.61 last year.
The cuts will impact all Part B therapy, with an additional impact if codes that were lowered in value (RVU) as part of the re-valuation noted above are of frequent use in your practice.
Did you know you can look up any CPT code and check the rate HERE ?
Other cuts currently in play? Oh so many….
- 15% cut for therapy services provided by assistants began in 2022 (CO/CQ modifiers)
- Multiple Procedure Payment Reduction (MPPR) of 50% to the Practice Expense of each CPT code for any subsequent unit of service performed after the first unit on the same day
- 2% Sequestration Cuts that were phased back in this July
- 4% PAYGO that was paused by legislation in 2022 coming back 2023
2. Virtual Services and Telehealth
Virtual Services is the umbrella category where Telehealth lives. Virtual Services encompass Telehealth, E-Visits, Virtual Check-Ins and Telephone E/M services.
Therapists were not able to provide telehealth services prior to the Public Health Emergency (PHE) and are currently only able to provide telehealth now through waiver authority under section 1135(b)(8) of the Act.
The ability for therapists to provide telehealth services after the waivers and interim policies expire was further extended in March of 2022, when Congress approved an extension of telehealth services for an additional 151 days after the PHE ends. This extension was included in the Consolidated Appropriations Act of 2022, allowing telehealth to continue a little bit longer in the SNF and other settings.
View the Act here, with attention starting on page 1901.
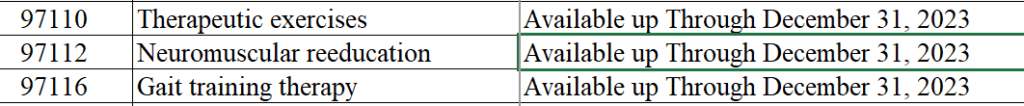
CMS provided the updated list of Telehealth CPT Codes for the PHE duration on 6/17/22. You can download the list here:
List of Acceptable Telehealth CPT Codes for PHE Duration (Zip file)
Of note, when viewing the list, even though some codes state “Available up through December 31, 2023,” therapist’s ability to bill for these codes will expire either PHE end + 151 days, or on 12/31/23, which ever comes first.
3. New Codes / Deleted Codes
Remote Therapeutic Monitoring:
Last year, 5 new codes were introduced for Remote Therapeutic Monitoring. For a detailed explanation of these, visit HERE. In the Proposed Rule, CMS seeks to replace 2 of those codes, 98980 and 98981.
- CPT code 98980 to GRTM3 ─ Remote therapeutic monitoring treatment management services, physician/ other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; first 20 minutes
- CPT code 98981 to GRTM4 ─ Remote therapeutic monitoring treatment management services, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; each additional 20 minutes
Chronic Pain:
CMS is proposing 2 new codes for the management of chronic pain. Though these codes will only be used by physicians / physician extenders, PT and OT collaboration is mentioned in the code description, which may allow a window for advocacy for our services in the future.
- HCPCS code GYYY1: Chronic pain management and treatment, monthly bundle including, diagnosis; assessment and monitoring; administration of a validated pain rating scale or tool; the development, implementation, revision, and maintenance of a person-centered care plan that includes strengths, goals, clinical needs, and desired outcomes; overall treatment management; facilitation and coordination of any necessary behavioral health treatment medication management; pain and health literacy counseling; any necessary chronic pain related crisis care; and ongoing communication and care coordination between relevant practitioners furnishing care (e.g., physical therapy and occupational therapy, and community-based care), as appropriate. Required initial face-to-face visit at least 30 minutes provided by a physician or other qualified health professional; first 30 minutes personally provided by physician or other qualified health care professional, per calendar month.
- HCPCS code GYYY2: Each additional 15 minutes of chronic pain management and treatment by a physician or other qualified health care professional, per calendar month
4. Direct Supervision by Interactive Telecommunications Technology
Currently, due to the PHE temporary rule set, the Medicare rule around supervision has been modified to include providing direct supervision via audio-visual technology. The Proposed Rule discussed the possibility of making this permanent policy, thus removing the need for direct supervision for Medicare reimbursement, though CMS is still seeking input on this.
CMS reminds us in the Proposed Rule that after December 31st of the year the PHE ends, pre-PHE rules for direct supervision would apply.
***Of note, this does not impact the SNF setting specifically as Medicare Part A and Part B in the SNF currently require “general supervision,” meaning a therapist does not need to be in the room or on site in order for an assistant to provide services. Medicare Part B supervision rules for Private Practice, however, are more strict, requiring “direct supervision.”
It is important that this rule is not confused with your State Practice Act requirements for supervision. Even though Medicare has temporarily relaxed the supervision regulation, if your State Practice Act for your particular therapy discipline requires on-site supervision, the Medicare rule is overridden.
5. Modifiers and Manual Medical Reviews
CO and CQ Modifiers for Assistant Services
We are finishing up year 1 of the impact of the 15% payment reduction for therapy services provided by an assistant that meet the CMS definition of “in whole or in part,” and are coded with the CO or CQ modifier. There are no changes proposed in this area. If you need a refresher to ensure you are using the modifiers correctly, visit HERE.
KX Modifier Threshold
The “old” Therapy Cap is now disguised as the KX Modifier Threshold, and “threshold amounts” change yearly. The 2022 “threshold” is $2150 for OT, $2150 for PT and Speech combined. We can expect a slight increase (~$40) for 2023 and will receive the official amount in the Final Rule. Continued use of the KX modifier is required for all therapy services that “would have exceeded the previous therapy cap amounts,” or claims will be automatically denied.
Manual Medical Review
The manual medical review threshold continues at the same amount of $3000 until 2028.
A review is not automatic when the $3000 is reached. CMS is using targeted reviews, limiting reviews to “outliers” and those with questionable practice patterns.
Important Links and Resources
Proposed Rule Federal Register Link
CMS Physician Fee Schedule Home Page
In Summary
Cuts, cuts and more cuts seem to be the theme for 2023…..and 2022…..and 2021…..
Remember, these changes are for Part B therapy only, and specific to the SNF setting. We teased out the parts of the Rule that applied to the SNF….so don’t worry about MIPS or other rules specific to private practice!
As always, if you have any questions about the information or how it will impact you, send them to us here: Just Ask Q&A
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team