Will your State use the Optional State Assessment (OSA) beginning on 10/1/23?
On April 24, CMS posted the Optional State Assessment (OSA) Item Set, OSA Manual, and OSA Change History table on CMS.gov, effective for use 10/1/23.
The OSA, a non-Federally required standalone assessment, was first released with the Final Minimum Data Set (MDS) Item Sets to begin 10/1/2019, to allow State Medicaid agencies to calculate the Resource Utilization Groups, RUG III or RUG IV, HIPPS codes for payment purposes.
Multiple sections on the MDS, in particular, Section G, were slated to be retired on 10/1/2020 which would have prevented the ability to calculate a RUG score. However, multiple factors came into play in 2020, including State Agencies begging for more time to gather data, and the COVID-19 Public Health Emergency, to name a few, and ultimately the decision was made not to proceed with the removal of items from the Federally required (OBRA) MDS assessments just yet.
Instead, CMS updated the MDS Item Sets to include Section GG on OBRA assessments for states that wanted to collect PDPM information, while still getting the RUG score needed for State Medicaid. This change allowed State Medicaid Agencies to collect and compare RUG-III/IV payment codes to PDPM ones, to inform their future payment models when Section G ultimately disappeared. However, all states did not select this option at the time, and to date, do not have comparable PDPM/RUG data.
Acting on a prior promise, CMS issued letters to State Medicaid Coordinators last September making it official that CMS would no longer support the Medicare RUGs systems after October 1, 2023, and would remove questions from federally required assessments (Admissions, Annuals, Quarterlies, Significant Change MDS) needed to generate a RUG-III and/or RUG-IV score. In the letter, CMS outlined options for States to transition to a PDPM-based model, or determine if they would temporarily continue with an unsupported RUG model.
Finally!
When we recently received the Final Item Sets that were to go into effect 10/1/2023, the OSA was not there which led to a bit of panic, as this would prevent any state from collecting RUG scores after October 1st. However, in the 2 previous SNF Open Door Forum calls, CMS assured participants that the OSA was going to be released as a separate MDS package.
Sure enough, 3 days ago CMS released the OSA package, with important links to the MDS Assessment form and the new 46 page OSA Manual here:
Of note, the only difference from the original 2019 OSA and 2023 OSA can be found in the Ethnicity / Race Sections, which have been expanded to mirror the modified OBRA sections on the new MDS effective 10/1/23. Other than that, the questions are the same.
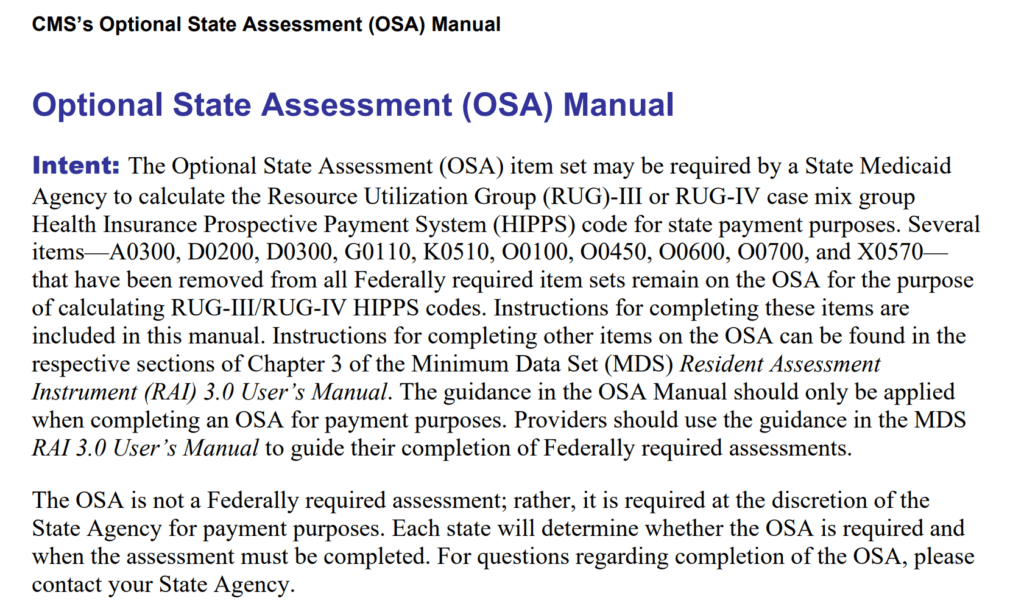
The introduction to the OSA Manual explains the intent of the Assessment.
The OSA contains only the Item Sets necessary to calculate a RUG III or RUG IV score, so it’s important to know what RUG version your State uses, and the questions that correspond to that RUG version.
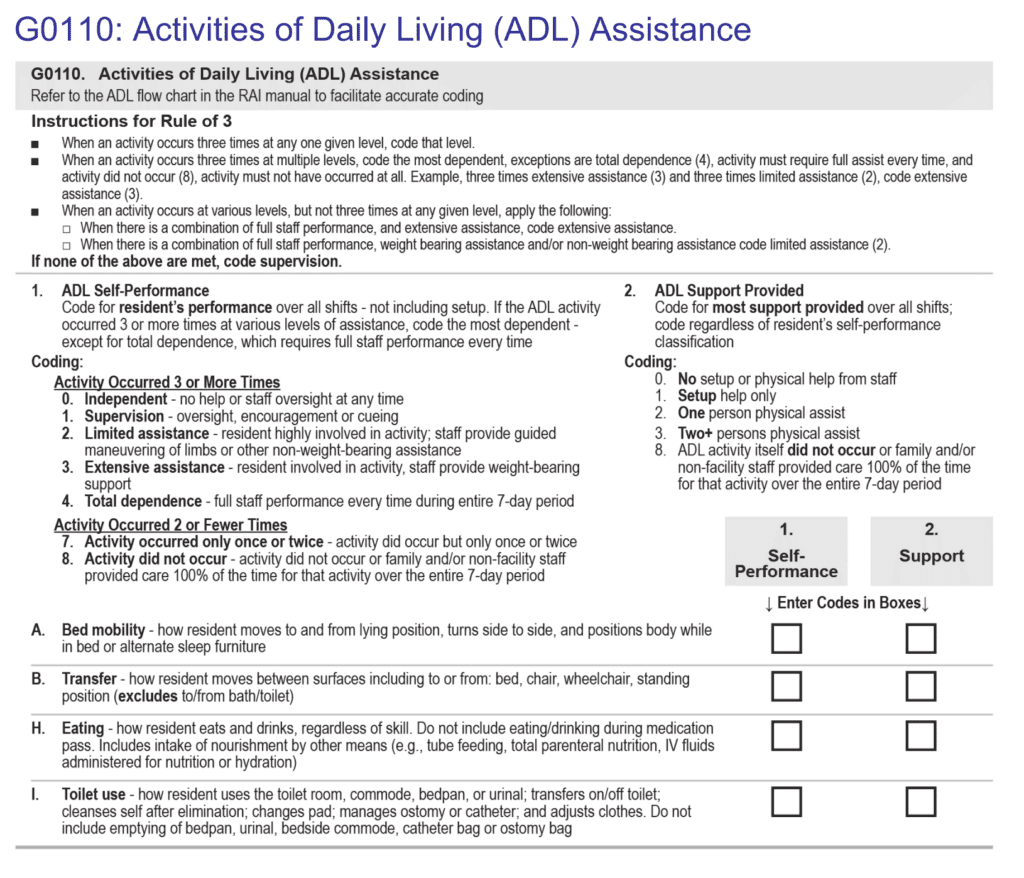
As you can see, Section G ADLs is short and sweet, with only the 4 late loss ADL questions needed to determine the ADL score.
Check in With Your EMR
There are a long list of questions that need to be sorted out prior to 10/1/23.
How will your software vendor support this transition? The RUG-III and RUG-IV score currently generated by current OBRA assessments (Quarterly, Annual…) will no longer be possible. OBRA assessments will only produce a PDPM HIPPS score. That’s it.
The OSA should be available on all EMR menus, though this may require set up with your vendor to enable this.
Additional items to clarify with your EMR:
Will the daily documentation flow for direct care staff change? Each shift typically documents on each Activity of Daily Living (ADL) domain by “clicking” how the resident performed on each task. These tasks have historically mirrored Section G MDS questions, and data was used for the algorithm to determine proper MDS coding of Section G using “the rule of three.” Now that Section G will not be on any federally required assessments, only existing on the OSA, what options does your EMR have for your? Facilities using the OSA will need to support both Section G (for OSA) and Section GG (for all Federal assessments).
If your State will be using RUGs for Medicaid payment, daily documentation to support the RUG will still be required. Make sure documentation options for “the old Section G items” is left untouched. It’s possible that your EMR may even be able to tie the daily documentation/ADL coding results into the OSA to calculate the ADL score. Can you imagine having to calculate the “rule of 3” for each ADL for each resident and enter the result manually? Or having to collect paper documentation to support the RUG?
It’s likely EMRs may be adding daily documentation options for direct care nursing staff (aides) to input all of Section GG Self Care and Mobility (though this may not be the best decision for PDPM outcomes…that’s a discussion for another day). Ensure Section G will remain, at least for the 4 late loss ADLs. You are going to need it on an OMIG audit.
Ultimately, there are multiple procedural items to work out with your EMR vendor for this transition, as software vendors will have to potentially make different adaptations for each State’s specific requirements and facility preferences, potentially increasing costs.
The first step is to nail down what exactly your state plans to do on 10/1/23.
Contact Your State RAI Coordinator
The OSA MDS and the corresponding Manual are now in place for 10/1/23. The final step is to get direction from your individual state. Will your state be transitioning to a PDPM payment methodology, continuing to collect RUG scores, “freezing” the current CMI score for a period of time while getting preparations into place? Or something else?
The CMS letter to States referenced above stated:
“CMS will no longer support the Medicare RUGs systems after October 1, 2023. CMS is available to assist states as Medicare RUGs transition to PDPM. Initial readiness determinations should be made by the states in collaboration with their provider communities. States that decide to transition to PDPM for purposes of Medicaid payment and UPL demonstrations should carefully review their currently approved state plan benefits and payment methodologies, as well as their UPL demonstration methodology for nursing facility services. States that include references to RUGs in the state plan and wish to change their payment methodologies to be based on Medicare PDPM or a different payment system must conduct public process and notices in accordance with statute and regulation and submit a state plan amendment to CMS for approval.“
September 2022 CMS Letter to States
Based on this language and the fact that 10/1/23 is less than 6 months away, states transitioning to PDPM should have already “conducted public process and submitted a state plan amendment to CMS for approval.” Has this happened in your state?
Your best bet may be to reach out to your State RAI Coordinator (repeatedly) over the next few months.
Here is a list of the State RAI Coordinators, updated April 2023, with names and email addresses. Reach out and see if they know what’s happening.
Link to State RAI Coordinators – Names & Email for Each State
PDPM or RUGs?
Whether states are planning on transitioning to PDPM or continuing with the RUG system for State Medicaid reimbursement, there needs to be time for facilities to train staff and set up new processes.
All SNFs will transition to PDPM eventually, as CMS indicated the OSA will remain until 10/1/25 and will then be retired.
In the meantime:
Facilities continuing with RUGs will have double the amount of MDSs for their Medicaid residents.
Facilities that will continue to use RUGs need to keep in mind that the MDS staff will now have additional MDSs to complete. There is no copy and paste solution here. The new OBRA MDS does not have a majority of the OSA questions, so it is not a matter of copying a quarterly to create an OSA.
There will be at least 1 additional MDS for each Medicaid resident per quarter.
States continuing with RUGs still have their work cut out for them.
Since the OSA is not Federally required and there are no parameters for when it is to be completed, States are going to have to set those regulations.
- When will the OSA need to be completed?
- How often will the OSA need to be completed?
- Can each resident have multiple OSAs in the CMI window? or only 1?
- How will States verify that each Medicaid resident had an OSA completed? Were the PA1 scores accidentally omitted?
- How will the final Medicaid CMI score be calculated? An average of all OSAs? One OSA per resident?
Not only will states need to coordinate the OSA guidelines, they will need to coordinate how to pull the assessment data from CMS. Remember, all the OBRA assessments will soon have PDPM HIPPS, not RUG scores. Can the state software pull only the OSA RUG scores?
Bottom line is that either RUGS or PDPM, states and facility staff have lots to prepare for to ensure a smooth transition, and that assessments reflect the most accurate case mix index of the facility Medicaid population.
What is your state doing? If you know, leave a note in the comments, as it may help one of your peers.
We will all know soon enough!
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA