The new Caregiver Training Service (CTS) codes have been in effect for over 1 month now, and their use is starting to pop up in chart reviews. Has your skilled nursing facility (SNF) therapy department had the opportunity to use them yet?
What are the 3 new Current Procedural Terminology (CPT) Codes?
- CPT code 97550, face-to-face with caregiver, without patient present
- Initial 30 minutes
- Caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community
- (e.g., activities of daily living, instrumental ADLs, transfers, mobility, communication, swallowing, feeding, problem solving, safety practices)
- CPT code 97551, face-to-face with caregiver, without patient present
- Each additional 15 minutes (used only after 97550 30-minutes is billed)
- CPT code 97552, face-to-face with caregivers representing more than 1 patient, without patient present
- Group caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community
- (e.g., activities of daily living, instrumental ADLs, transfers, mobility, communication, swallowing, feeding, problem solving, safety practices)
Why are these codes unique?
- These CTS codes are the first of their kind for therapy, as they are intended for use without the resident present. Therapy CPT codes in use up to this point require the resident to be present (direct contact), and any caregiver training that occurs is billed under the most appropriate CPT code that the training falls under (ADL, gait, therapeutic exercise).
- Codes are defined as face-to-face training with the caregiver
- Center for Medicare & Medicaid Services (CMS) has defined “caregiver” “as:
- “an adult family member or other individual who has a significant relationship with, and who provides a broad range of assistance to, an individual with a chronic or other health condition, disability, or functional limitation”
- “a family member, friend, or neighbor who provides unpaid assistance to a person with a chronic illness or disabling condition”
- Written consent is required from the resident to approve the training in their absence. If the resident is unable to consent, the consent of the resident representative is required.
- All CTS codes are not billed using the typical 15-minute unit structure
- The CTS code-set contains its own “group” code, differing from the 97150 CPT Group Code used for treatments that meet the definition of group therapy
When would these codes be used?
In the Physician Fee Schedule (PFS) Final Rule for CY 2024, CMS provided a framework for usage of the CTS codes.
- “These codes are for when the treating practitioner identifies a need to involve and train one or more caregivers to assist the patient in carrying out a patient-centered treatment plan.” In other words, when the resident is not able to independently carry out necessary components of the treatment plan and/or discharge plan.
- “The goals and outcomes of the sessions focus on interventions aimed at improving the patient’s ability to successfully perform ADL’s”……”to facilitate the patient’s functional performance in the home or community”
- “Caregivers are taught how to facilitate the patient’s activities of daily living (ambulating, feeding, dressing, personal hygiene, continence, and toileting), transfers, mobility, communication, and problem-solving to reduce the negative impacts of the patient’s diagnosis on the patient’s daily life and assist the patient in carrying out a treatment plan.”
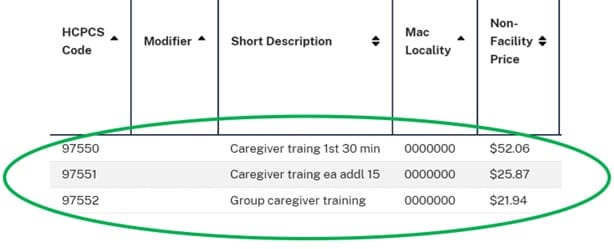
What is the reimbursement for the cTS Codes?
These are the National Rates from the CMS CPT look-up tool for CY2024:
| CPT Code | Name / Description | Amount (“Non-Facility” Price for SNF) |
| 97550 | Caregiver Training – Face to Face – 30 minutes | $52.06 for 30 minutes |
| 97551 | Caregiver Training – Face to Face – Each additional 15 minutes | $25.87 for additional 15 minutes |
| 97552 | Group Caregiver Training – Face to Face – Untimed | $21.94 billed to each resident in group |
Directions on how to use the CPT look-up tool
How do these rates compare to other common CPT codes used in the SNF?
Using the National Rates for CY2024, the non-group Caregiver Training codes (97550 and 97551) average $25 for 15 minutes, falling slightly under the per unit rates for the 97000 timed codes listed below. Swallowing therapy, CPT 92526 is an untimed code, paying a flat rate per day.
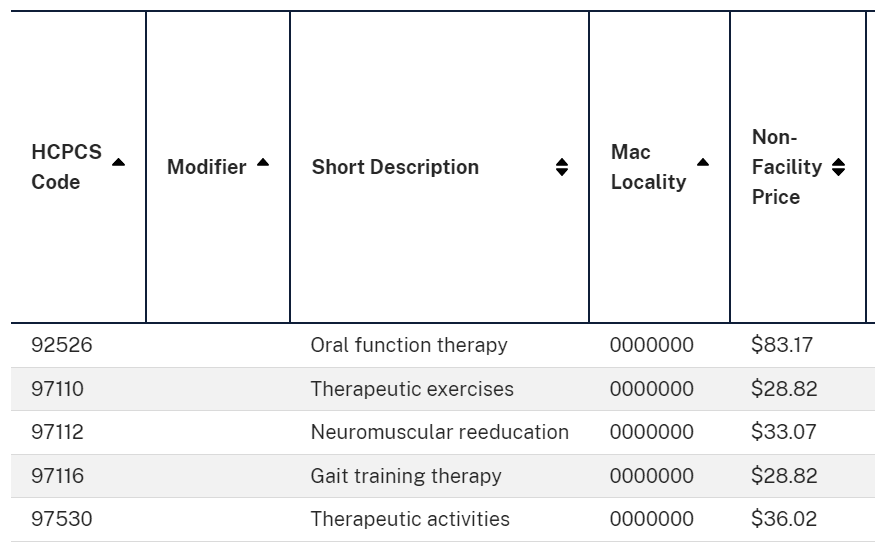
Use the CMS CPT look-up tool to get the exact rates for your location by entering your Medicare Administrative Contractor MAC).
real sNF Billing Scenarios
It is important to remember that these codes apply to all settings where Medicare Part B is billed, and usage may be more appropriate in some settings than others.
Here are a few SNF scenarios gathered from recent chart reviews.
- Teaching total hip precautions to a caregiver of a resident who cannot comprehend the restrictions, and is in too much pain for therapist to mobilize for the demonstration. Precautions are taught to the caregiver for carryover upon discharge home. Caregiver was also instructed in the need to adjust seating surface height in the home in preparation for resident discharge. Caregiver was provided with verbal and written instructions, and pictures of do’s and don’ts for hip precautions.
- Instructed caregiver in car transfers for resident who had recent stroke with hemiparesis with goal of discharge home. Caregiver requires demonstration on how to transfer resident from wheelchair to car, including proper set up, management of car door and wheelchair parts. Caregiver would benefit from car training with staff prior to introducing resident to the situation, due to resident high anxiety. Training using therapist in place of resident and verbally instructing caregiver throughout transfer to insure competence and safety prior to caregiver training with resident and caregiver’s car.
- Group caregiver training session for caregivers of 3 separate residents on need for and use of thickened liquids due to history of aspiration. Caregivers will be preparing meals/liquids upon discharge home. Group training to review aspiration precautions, how to prepare modified meals/liquids, review of signs and symptoms for concern. Caregivers received verbal, written and video instruction.
Do these situations meet the Caregiver Training Service code definitions?
But, but, but what about…..???
- Does Medicare Part B actually reimburse for these codes? Yes – See above rates
- Do other payors reimburse for them? Depends – Check individually
- Can PTA and OTA (assistants) use these codes? Yes
- Can these codes be used for telehealth? No
- Do we need written consent from the resident? Yes
- What if the resident is unable to consent? Ask responsible party
- Can time educating caregivers in care conferences count? No
- Can you use the individual and group codes in the same day? Yes
- Is a nurse or nurse aide a caregiver? No – See definition of caregiver above
- Can the minutes be counted on the MDS? Some debate exists.
- CTS codes came out after last RAI Manual update 10/1/23
- Billing codes required resident direct contact prior to these new codes
- New codes meet definition of skilled therapy if parameters are met
- Question is “Do these codes meet the therapy mode definitions?”
- Section O states: “Record total number of minutes therapy administered to the resident individually…..” Since resident was not present, can minutes be counted? To date, there is no written clarification.
- Using the logic that CTS codes came later, and in these scenarios the caregiver is an extension of the resident, which the resident has consented to in writing, these skilled therapy minutes should qualify for recording on the MDS.
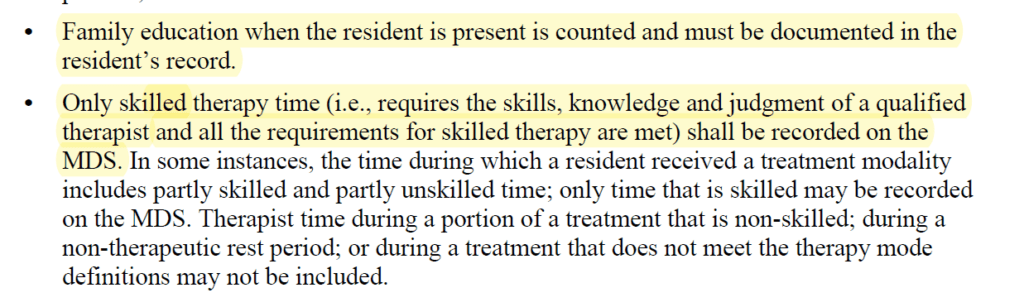
- See current RAI Manual excerpt below and use your best judgement until clarified by CMS. The second bullet should guide your decision-making.
RAI Manual Chapter 3, Page O-24 “Minutes of Therapy”
In Summary
Based on the requirements of these new codes, this type of caregiver training should not be routine for all residents; therefore, it should not be in every single plan of care.
When the need for involving a caregiver in training is identified by the treating practitioner (ie: not the person in charge of doing the schedule), it should be documented on the evaluation or in a later document, outlining why this type of training is required and why the resident need not be present.
In the SNF setting, there will likely be more instances of caregiver training with the resident present vs without, and in those instances, we should continue to document and bill as we have been for years, under the corresponding CPT code that covers the topic of training.
Most importantly, note that built into the code definitions is the verbiage “…to facilitate the patient’s functional performance in the home or community.” This suggests that usage of these codes is geared toward residents with a discharge plan to the community, and would need special justification for routine use with long-term care residents.
As always, if you have any questions about the information or how it will impact you, send them to us here: Just Ask Q&A
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Resource Team
MonteroTherapyServices.com