CMS released the Physician Fee Schedule (PFS) Final Rule yesterday, a.k.a. the “Medicare Part B Rule,” outlining changes for 1/1/24. After reviewing thousands of comments submitted by providers since the Proposed Rule release, CMS made some minor changes.
This 2,709-page document includes information on payment rate changes, new codes, supervision of assistants, telehealth and more! We highlighted the Medicare Part B rules that impact therapy in the SNF setting.
Final Changes For January 1st, 2024
1. Rate Information
Rate cuts have been the norm in recent years, and 2024 will be no different. CMS is proposing a 3.4% decrease in the Conversion Factor, resulting in a 1.25% decrease in overall payments under the Physician Fee Schedule (PFS) as compared to CY 2023, according to the CMS Fact Sheet.
The 3.4% Conversion Factor cuts for CY 2024 are in part due to the expiration of the 2.5% “intervention” from Congress ending 12/31/23, a budget neutrality adjustment, and a 1.25% increase from Congress to offset the cuts.
**[Edited March 2024 after additional government funding package released: “On March 8, Congress passed a 2nd adjustment that contained a reduction of approximately half, eliminating 1.68% of the 3.37% cut to the Medicare Physician Fee Schedule that went into effect January 1, 2024.”]
Cuts explained….
Cuts can be attributed to a decrease in the Conversion Factor (CF). This is a value that CMS modifies yearly, and is part of the formula that determines the dollar amount for each CPT code by converting Relative Value Units (RVU). The CF impacts all Current Procedural Terminology (CPT) Codes across the board. When the CF decreases, the overall payment rate for the CPT codes decrease, unless the RVU for a specific CPT code is increased enough to offset the CF drop.
The CF has not been trending in a favorable way over the past 5 years, and will drop from $33.89 last year to $32.74 for CY 2024.
Did you know you can look up any CPT code and check the reimbursement rate HERE ?
2. Telehealth
As we are all well aware of, therapy professionals were not able to provide telehealth services prior to the Public Health Emergency (PHE) and are currently only able to provide telehealth now post-PHE, through a temporary continuation of these extended flexibilities outlined in the Consolidated Appropriations Act of 2023.
The Act affirmed the extension of telehealth flexibilities through 12/31/24, and the Final Rule confirmed that the SNF setting is included in this extension.
The Proposed Rule indicated a change with the Place of Service (POS) codes on the claim when billing telehealth services. These changes were confirmed in the Final Rule, along with a clarification from CMS for outpatient therapy providers, explained below:
During the PHE, providers were instructed to use Modifier 95 on the billing claim to indicate telehealth, and the Place of Service (POS) code to indicate “where the services would have occurred had it not been furnished via telehealth.” This allowed telehealth services to be paid at the higher non-facility rate during the PHE. For CY2024, CMS indicated in the Proposed Rule that Modifier 95 would no longer be used, and providers would transition back to using POS codes that represent the actual location. The original POS Code to indicate telehealth, “02,” has been redefined, and a new POS Code, “10,” has been created. Each POS code will indicate different location and reimbursement rates.
● POS “02” – Telehealth Provided Other than in Patient’s Home: Used when patient is not in their home when receiving services. Will be paid at the Facility PFS Rate.
● POS “10” – Telehealth Provided in Patient’s Home: Used when patient is located in their home (not facility). Will be paid at the Non-Facility PFS Rate.
While the above transition will be in effect for most providers, in the Final Rule, CMS clarified the following for therapy services:
“We wish to clarify that, for outpatient therapy services furnished via telehealth by PT, OT, or SLP distant site practitioners, the furnishing practitioner should continue to append the 95 modifier to identify them as telehealth services rather than a telehealth POS code.
Page 160 Final Rule
We also note that payment will continue to be made for telehealth services furnished by distant site PTs, OTs, or SLPs through the end of CY 2024, and that these services will continue to be paid the non-facility rate.
CMS provided the updated list of Telehealth CPT Codes for CY2024 that can be accessed here:
Download CY 2024 List Of Telehealth Acceptable CPT Codes (Updated 11/2/23)
If the CPT code is not on the telehealth list from CMS, the service can not be provided via telehealth. The list of codes can be downloaded above, or viewed on pages 140-144 of the Final Rule.
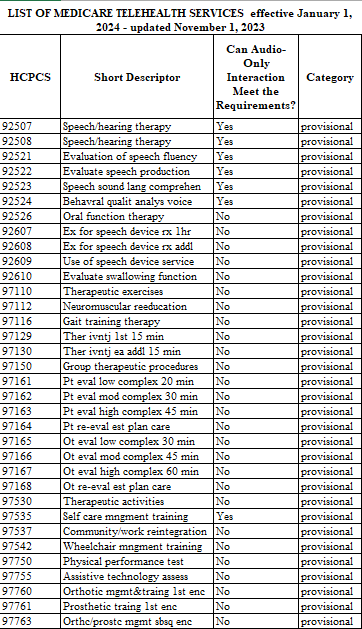
Listed here from the Rule are approved telehealth CPT codes frequently used in the SNF setting include:
3. New Codes / Adjusted Codes / Deleted Codes
New Codes!
Caregiver Training Services (CTS)
CMS finalized 3 new codes for CTS under a PT, OT or Speech plan of care when the treating practitioner identifies a need to involve and train one or more caregivers to assist the patient in carrying out a patient-centered treatment plan.
- CPT code 97550
- Caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community (e.g., activities of daily living, instrumental ADLs, transfers, mobility, communication, swallowing, feeding, problem solving, safety practices)
- without the patient present
- face-to-face; initial 30 minutes
- CPT code 97551
- Each additional 15 minutes; List separately in addition to 97550
- CPT code 97552
- Group caregiver training in strategies and techniques to facilitate the patient’s
functional performance in the home or community (e.g., activities of daily living, instrumental ADLs, transfers, mobility, communication, swallowing, feeding, problem solving, safety practices) - without the patient present
- face-to-face with multiple sets of caregivers (training involves >1 patient)
- Group caregiver training in strategies and techniques to facilitate the patient’s
CMS Definition of Caregiver
There are 2 unique details about these codes. First, the resident is not present for the training, and second, the term “caregiver” is a CMS-defined set of individuals, and does not include paid caregivers of the facility, such as nurse aides.
After considering public comments, CMS finalized an expanded definition of caregiver as:
“An adult family member or other individual who has a significant relationship with, and
Final Rule, page 294
who provides a broad range of assistance to, an individual with a chronic or other health
condition, disability, or functional limitation” and “a family member, friend, or neighbor who
provides unpaid assistance to a person with a chronic illness or disabling condition”.
Regarding training that occurs without the resident present, CMS further adds:
“Although the patient does not attend the trainings, the goals and outcomes of the sessions focus on interventions aimed at improving the patient’s ability to successfully perform activities of daily living (ADL’s). Activities of daily living generally include ambulating, feeding, dressing, personal hygiene, continence, and toileting. During the face-to-face service time, caregivers are taught by the treating practitioner how to facilitate the patient’s activities of daily living, transfers, mobility, communication, and problem-solving to reduce the negative impacts of the patient’s diagnosis on the patient’s daily life and assist the patient in carrying out a treatment plan.”
Takeaways for use of these new codes…
- Treating practitioners have to identify the need to involve and train a caregiver to assist in carrying out a treatment plan.
- These are planned and coordinated training sessions. The need for this type of training must be identified in the therapy plan of care.
- This type of training should not be routine for all residents. Remember, it is provided when training does not require the resident to be present.
- CMS confirmed in the Final Rule that documented consent from the resident (or representative if the resident is unable), is required to carry out this training without them.
Remember, coding caregiver training for facility staff (ie: nurse aides) and resident’s family with the resident present is different from the above new codes, and should continue to be provided. These interactions will continue to be billed under the corresponding CPT Code that covers the topic of training. (ie: ADL, Therapeutic Activities, etc.)
Adjusted Codes
Remote Therapeutic Monitoring (RTM)
In 2022, 5 new codes were introduced for Remote Therapeutic Monitoring. For a detailed explanation of these, visit HERE. In the Final Rule, CMS refined some aspects of these codes, and also offered a correction from the Proposed Rule regarding which CPT codes the changes applied to.
As of the end of the PHE, the RTM rule changed and the 16-day monitoring requirement was reinstated, meaning, monitoring must occur over at least 16 days of a 30-day period. The Proposed Rule made a general statement about the new rule application to all codes. However, the Final Rule clarified that the 16-day requirement does not apply to CPT Codes 98980 and 98981 (page 185).
The following remote monitoring codes, however, require collection of no fewer than 16 days of data in a 30- day period, as defined and specified in the code descriptions:
- 98976 (Remote therapeutic monitoring (eg, therapy adherence, therapy response); device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to
monitor respiratory system, each 30 days); - 98977 (Remote therapeutic monitoring (eg, therapy adherence, therapy response); device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to
monitor musculoskeletal system, each 30 days); - 98978 (Remote therapeutic monitoring (eg, therapy adherence, therapy response); device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to
monitor cognitive behavioral therapy, each 30 days)
The Final Rule also clarified that PTAs and OTAs in private practice can provide the service under “general supervision” vs direct through 12/31/24. (Pages 494-496)
Therapy Codes That May Get A Pay Increase
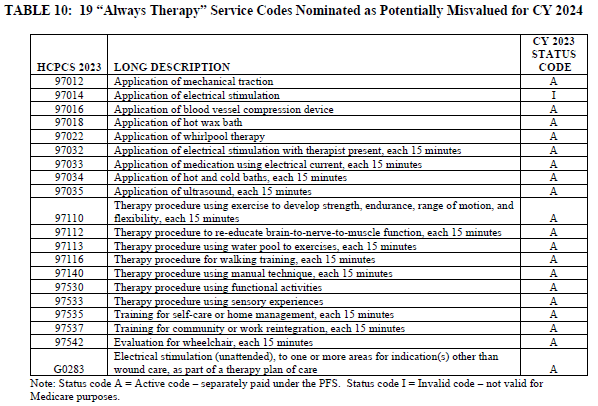
19 CPT Codes used by PT and OT were finalized to “consider as potentially misvalued codes for CY2024.” This means that the codes will be reviewed for an increase in reimbursement. The codes are listed below:
4. Direct Supervision By Interactive Telecommunications Technology
The Medicare rule around supervision was modified during the PHE to include providing direct supervision via audio-visual technology. Throughout the PHE and to this date, there have been discussions of potentially making this shift in supervision of the PTA/OTA permanent policy. However, for now, the rule remains temporary.
For CY2024, CMS clarified that the PHE requirement of direct supervision through virtual presence using audio/video real-time communication technology, will remain through 12/31/24.
“We believe that extending this definition of direct supervision through December 31, 2024, would align the timeframe of this policy with many of the previously discussed PHE-related telehealth policies that were extended under provisions of the Consolidated Appropriations Act of 2023.”
CMS also clarified the requirement of direct supervision through virtual presence using audio/video real-time communications technology “could be met by having the supervising practitioner be immediately available to engage via audio/visual technology,” and “would not require real-time presence or observation of the service.”
This will continue through 12/31/24.
Two important points here:
1- This does not impact the SNF setting specifically, as Medicare Part A and Part B in the SNF require “general supervision,” meaning a therapist does not need to be in the room or on site in order for an assistant to provide services. Medicare Part B supervision rules for Private Practice require “direct supervision.”
2- The requirements of your State Practice Act may be more strict than Medicare’s temporary definition change. Even though Medicare has temporarily relaxed the supervision regulation, if your State Practice Act for your particular therapy discipline requires on-site supervision, the Medicare rule is overridden.
5. Modifiers And Manual Medical Reviews
CO and CQ Modifiers for Assistant Services
We are finishing up year 2 of the impact of the 15% payment reduction for therapy services provided by an assistant that meet the CMS definition of “in whole or in part.” There are no changes proposed for the CO or CQ Modifiers. If you need a refresher to ensure you are using the modifiers correctly, this will help.
KX Modifier Threshold
The “old” Therapy Cap is now disguised as the KX Modifier Threshold, and “threshold amounts” change yearly. The 2023 “threshold” of $2,230 for OT, $2,230 for PT and Speech combined, will increase to $2,330 for CY2024. Continued use of the KX modifier is required for all therapy services that “would have exceeded the previous therapy cap amounts,” or claims will be automatically denied.
The KX Modifier is an attestation by the therapist that the resident continues to require medically necessary services beyond the dollar threshold, and the rationale for the extended therapy services are documented in the medical record. All therapists should be aware of the amount of therapy a resident has received in a calendar year, and if over the threshold during a current episode of care, documentation should focus on supporting the extended services.
Manual Medical Review
The manual medical review threshold continues at the same amount of $3,000 until 2028.
A review is not automatic when the $3,000 is reached. CMS is uses the Targeted Probe and Educate (TPE) review process with providers identified through data submission as “outliers.” The TPE looks for providers with questionable practice patterns and provides training to decrease the error rate. For more information on the TPE process, visit the CMS info page or check out the Q&A Document.
Important Links And Resources
Federal Register Copy (Available 11/16/23)
In Summary
A few bright spots are mixed in with the cuts this year, with 3 new codes for Caregiver Training joining the 97000 family, 19 PT and OT common CPT codes that may “receive a raise,” and the ability for therapy professionals to provide telehealth in the SNF through 12/31/24.
Remember, these changes are for Part B therapy only, and specific to the SNF setting. We teased out the parts of the Rule that applied to the SNF….so don’t worry about MIPS or other rules specific to private practice!
As always, if you have any questions about the information or how it will impact you, send them to us here: Just Ask Q&A
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team
MonteroTherapyServices.com