CMS released the Medicare Part A Skilled Nursing Facility Prospective Payment System (SNF PPS) FY2022 Proposed Rule this week. The Rule contains the components that will go into effect 10/1/21 pending any changes made based on comments and feedback over the next few months. We discussed the “usual” details of the Proposed Rule, including rate changes, ICD-10 mapping changes for the Patient Driven Payment Model (PDPM) and more, in a separate article titled, “SNF Medicare Part A Proposed Rule for October 1st 2021 – Some Hidden Gems,” which can be found HERE.
In this article below, 2 of those “hidden gems” from the proposed rule are discussed….and they both involve therapy, $$, or both.
- How Did Therapy Provision Change from RUG-IV to PDPM?
- Was PDPM Budget Neutral in FY2020?
Chances are, you already know the answers to both questions…
How Did Therapy Provision Change from RUG-IV to PDPM?
CMS has stated in the past and reiterated again in this proposed rule, that they are monitoring SNF provider behavior under PDPM. CMS used this proposed rule as an opportunity to share “some [but not all] data” and made a point to show what they state as “clear evidence that PDPM alone, and not the PHE, is impacting certain aspects of SNF patient care provisions.”
This “clear evidence” of a change in provider behavior specifically refers to how much and what mode or type of therapy is provided, independent of the impact of the PHE.
CMS provided clear examples of therapy usage as follows:
Minutes of Therapy Per Day:
- Therapy volume through 9/30/2019: Average number of therapy minutes per day at 91
- Immediately after 10/1/2019: Average number of therapy minutes per day at 62
This pre-pandemic change showed a >30% decrease in daily therapy minutes for Part A residents.
Modes of Therapy:
- Pre PDPM % of SNF Stays With Concurrent and/or Group Therapy: 1%
- In the first month of PDPM, % of SNF Stays with Concurrent and/or Group Therapy: Concurrent 32%, Group 29%
This pre-pandemic change showed a 3,100% increase in concurrent, and a 2,800% increase group therapy.
CMS reports that “coincidentally, these numbers then dropped to 8% and 4%, respectively, beginning in April 2020 when the PHE was declared.” Even with the PHE and mandates for social distancing, the % of SNF stays using concurrent and/or group was significantly higher than pre-PDPM days! [Concurrent still up 700% and Group up 300%]
CMS noted that the increase of non-individual therapy was anticipated prior to PDPM implementation, and has addressed the expectation for one-on-one therapy to be the primary delivery method in prior Rules…remember the 25% threshold for group and concurrent? CMS repeated, again, in this proposed rule, that “the unique characteristics and goals of each SNF patient should drive patient care decisions, and financial motives should not override the clinical judgment of a therapist or therapy assistant or pressure a therapist or therapy assistant to provide less than appropriate therapy.”
CMS also noted that despite the changes in therapy provision, no significant changes in health outcomes were noted in the areas of falls with major injury, % of stays ending with Stage 2-4 or unstageable pressure ulcers or deep tissue injury, % of stays readmitted to an inpatient hospital setting within 30 days of SNF discharge, or other similar metrics. That’s not necessarily proof that changes did not happen, only that changes were not coded on an MDS.
CMS states they will continue to monitor these and other metrics to identify any adverse trends that may have been caused by changes in care patterns that accompanied the implementation of PDPM. Hopefully, CMS will share “the rest” of the data at some point.
Of note, all these changes in therapy provision did not directly impact PDPM payments, as there is no tie between therapy and case mix group scores under PDPM. However, providing less therapy or grouped therapy was undoubtedly a cost savings for SNFs and Rehab Providers alike.
Now let’s talk about payments.
Was PDPM Budget Neutral in FY2020?
PDPM was proposed and finalized to be implemented in a budget neutral manner. This means that the transition to PDPM was not intended to result in an increase or decrease in the aggregate amount of Medicare payment to SNFs.
Well? It was a repeat of what happened in FY2011 when SNFs transitioned from RUG-III to RUG-IV….. significant differences between what was expected and what actually happened with SNF PPS payments and case-mix utilization under. Oops.
CMS shared “some” data collected at the start of PDPM, and over the course of FY2020, that outlined significant practice pattern differences knocking PDPM off its’ budget neutral pedestal, that will result in a necessary “recalibration.”
- PDPM – What Was Expected
- PDPM was to be budget neutral, meaning that with the transition from RUG-IV to PDPM, the payment to SNFs would not increase or decrease. Factors and analysis used to determine the payment system rates for PDPM were made based on the assumptions that the resident population in the SNF would not change, provider behavior would not change, and coding practices would not change. The expectation for the transition year was that nothing would change.
- PDPM – What Actually Happened
- Significant differences between what was expected and what actualized at the start of PDPM in October 2019 occurred, significantly impacting CMS spending. Analysis (with removal of data specific to COVID-19) showed a 5% increase in aggregate spending under PDPM.
- Change in SNF behavior, in particular, coding practices impacting the Speech, Nursing and Non-Therapy Ancillary Components. No specific examples were given for MDS coding changes that were not anticipated, though items such as speech co-morbidities, cognitive impairments, swallowing issues, modified diets, morbid obesity and malnutrition may have been a few of the contributing factors.
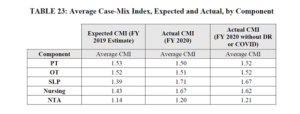
- How Much Did Speech, Nursing and NTA Change?
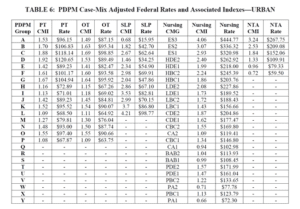
- The chart below identifies a 22.6% increase in Speech Case Mix Group scores, 16.8% increase in Nursing Case Mix Group scores, and 5.6% increase in NTA Case Mix Group scores for all Part A residents in FY2020 as compared to what was expected based on 2019 data analysis.
-
- CMS acknowledged that the public health emergency kicked in 5 months after the start of PDPM, and has looked at the data both with and without COVID-19 influence. The Case Mix Groups showed significant increases, even when adjusted to remove COVID-19 data.
- CMS ruled out COVID as a cause for the 5% increase in payments, and related the increase to the distribution in the CMG’s above, resulting from provider behavior changes.
Recalibration Method Proposed – Recalibrating the PDPM Parity Adjustment
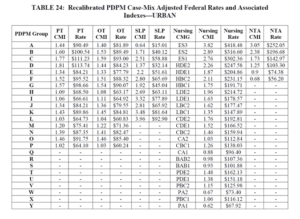
Since it doesn’t seem provider behavior is going to revert back to “as predicted,” the only other option is to “recalibrate.” CMS has included in the proposed rule for 10/1/2021, a potential recalibration of PT, OT, Speech, Nursing and Non-Therapy Ancillary Case Mix Index values, and a resulting adjusted Federal Daily Per Diem Rate.
Look at the 2 charts below.
The first, is the proposed PDPM Case Mix Adjusted Federal Rates (Urban) and CMI values, without recalibration.
The second, is the proposed potential recalibrated PDPM Case mix Adjusted Federal Rates (Urban) and adjusted CMI values.
The individual component rate decrease for each CMG from the proposed compared to the recalibrated are as follows:
- PT and OT rates decrease an average of $5 per day for each CMG
- Speech averages a $3 decrease per day
- Nursing rates decrease between $5-26 per day per CMG
- NTA rates decrease between $3-15 per day per CMG
Keep in mind that the recalibrated rates are not only lower than the proposed rates without the calibration, they are even lower than the rates currently in place…so we will be going backwards for sure! Comparing the recalibrated rates with today’s rates, a daily rate could range from $10-48 less….per day x 100 days for 1 resident! That’s a huge hit for all involved!
Recalibrations Happen
In the proposed rule, CMS outlines a potential recalibration method to address the issues presented above, with an attempt to restore the budget neutral manner that was intended. Recalibrations would possibly be introduced over time, as the financial impact would be significant. But it is clear that they will happen. The 5% increase needs to be recouped. CMS is seeking comments on a path forward for recalibrating the PDPM. Comments on recalibration or any aspect of the proposed rule can be made through June 7, 2021.
Because these “recalibrations” will impact the rates of the PT, OT, Speech and other PDPM Component Groups, SNF therapy professionals can start thinking about what kind of recalibrations might be felt on their end and how they can be handled. Contract Rehab Company therapists and in-house SNF therapy professionals may feel the recalibration differently, though both will surely feel the overall rate decrease.
Therapists are very familiar the “do more with less” undertone that kicked in with PDPM, and can only anticipate the impact on services if rates decrease further, all while trying to balance what is best for each resident. Do you have constructive comments or suggestions for CMS about the proposed rule? If so, here’s how to provide input:
- Electronically. You may submit electronic comments on this regulation to http://www.regulations.gov. Follow the “Submit a comment” instructions. In commenting, please refer to file code CMS-1746-P.
- By regular mail. You may mail written comments to the following address ONLY: Centers for Medicare & Medicaid Services, Department of Health and Human Services, Attention: CMS-1746-P, P.O. Box 8016, Baltimore, MD 21244-8016 [In commenting, please refer to file code CMS-1746-P]
- By express or overnight mail. You may send written comments to the following address ONLY: Centers for Medicare & Medicaid Services, Department of Health and Human Services, Attention: CMS-1746-P, Mail Stop C4-26-05, 7500 Security Boulevard, Baltimore, MD 21244-1850 [In commenting, please refer to file code CMS-1746-P]
- Inspection of Public Comments: All comments received before the close of the comment period are available for viewing by the public, including any personally identifiable or confidential business information that is included in a comment. We post all comments received before the close of the comment period on the following website as soon as possible after they have been received: http://www.regulations.gov. Follow the search instructions on that website to view public comments. CMS will not post on Regulations.gov public comments that make threats to individuals or institutions or suggest that the individual will take actions to harm the individual. CMS continues to encourage individuals not to submit duplicative comments. We will post acceptable comments from multiple unique commenters even if the content is identical or nearly identical to other comments.
Staying 1 step ahead of the rule changes is the best position to be in.
HERE is a link to the Proposed Rule. [PDF Copy HERE].
Read about all the other changes in the proposed rule HERE.
If you have any questions, send them to our Just Ask Q&A Forum and we will reach out to you to get your questions answered.
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team | www.MonteroTherapyServices.com