Centers for Medicare and Medicaid Services (CMS) released the Medicare Part A Skilled Nursing Facility (SNF) Prospective Payment System (PPS) FY2024 Proposed Rule last week containing the components that will go into effect 10/1/23 pending any changes made based on comments and feedback over the next few months.
The Proposed Rule provides updates to Part A rates, ICD-10 diagnosis code mapping for Patient Driven Payment Model (PDPM) calculations, SNF Quality Reporting Program (SNF QRP) changes, and SNF Value Based Purchasing (SNF VBP) updates. Based on the changes to the Quality Measures (QM) in this rule, it is evident that the focus continues to be on improving the quality of care and safety in the SNF setting.
With each year, the amount of information needed to share grows and grows. Now that the Public Health Emergency (PHE) is coming to an end, it seems that CMS is unleashing everything that has been delayed due to COVID-19. There is quite a bit of information to follow, and we teased out what is most pertinent to SNF therapy and MDS professionals. Take it 1 piece at a time.
Medicare Part A Payment Rate Changes
The Federal Per Diem rates are updated annually. On 10/1/23, the rates for Part A have a proposed net increase of 3.7%, or $1.2 billion in Medicare Part A payments to SNFs in FY2024. To put this in perspective, if all 15,000+ SNFs were created equal, this would equate to approximately $80,000 more per SNF.
Medicare Part A rate updates will include “Phase 2” of the PDPM parity adjustment recalibration, required to “right the wrongs” of provider practice patterns that occurred during the first year after transition from the RUG-IV payment system to the PDPM, that caused a 5% overpayment to SNFs. In FY2024, SNFs will be “paying back” the remaining 2.3%.
The rate increase detail: [(Market Basket % increase of 2.7% + Forecast Error Correction of 3.6%) – 0.2% Multi-factor Productivity Adjustment (MFP)] = 6.1%, further reduced by 2.3% reduction for the PDPM recalibration, resulting in a “net increase of 3.7%” per CMS.
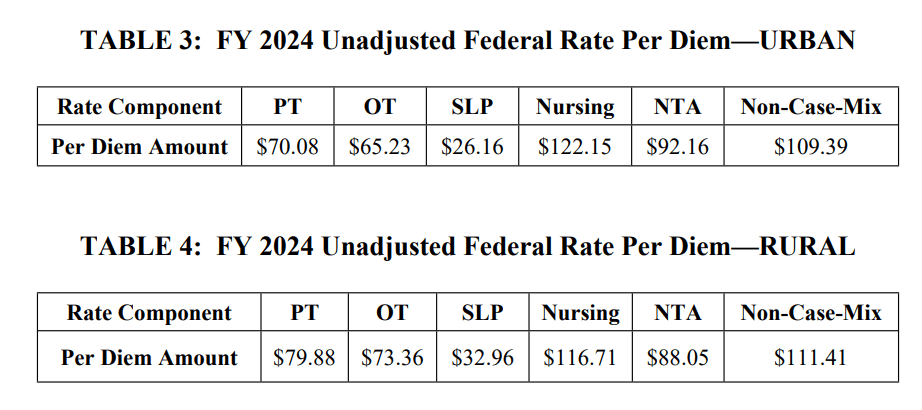
Below are the proposed unadjusted rates, that when multiplied by the case mix index values, determine each PDPM Case Mix Group rate.
Medicare Part A PDPM Changes – Case Mix Index Values
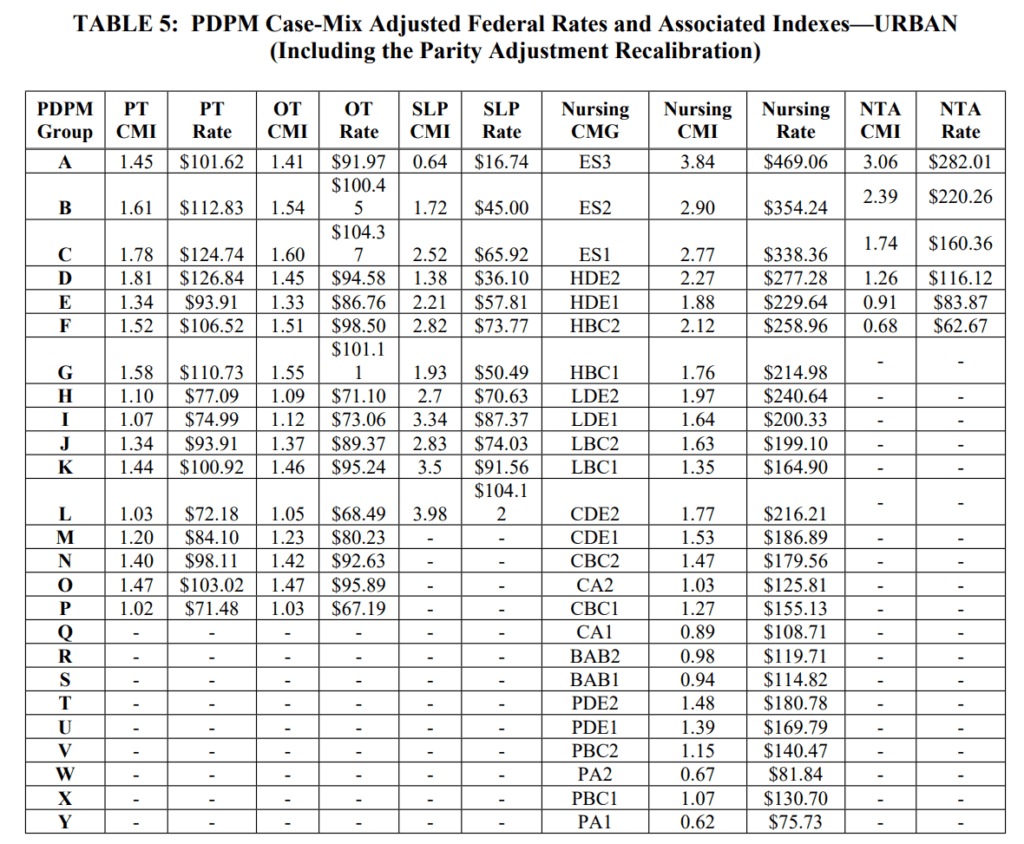
Case Mix Index (CMI) values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, showed significant reductions last year, and will remain the same for FY2024. Adjusting the CMI values is how the “PDPM recalibration” is accomplished, producing overall lower Medicare Part A rate payments per day. When multiplied by the Unadjusted Federal Per Diem Rates shown above, Case Mix Group rates will look something like this for FY2024.
Proposed FY2024 (Urban)
Medicare Part A PDPM Changes – ICD-10 Code Mapping for PT, OT and Speech Components
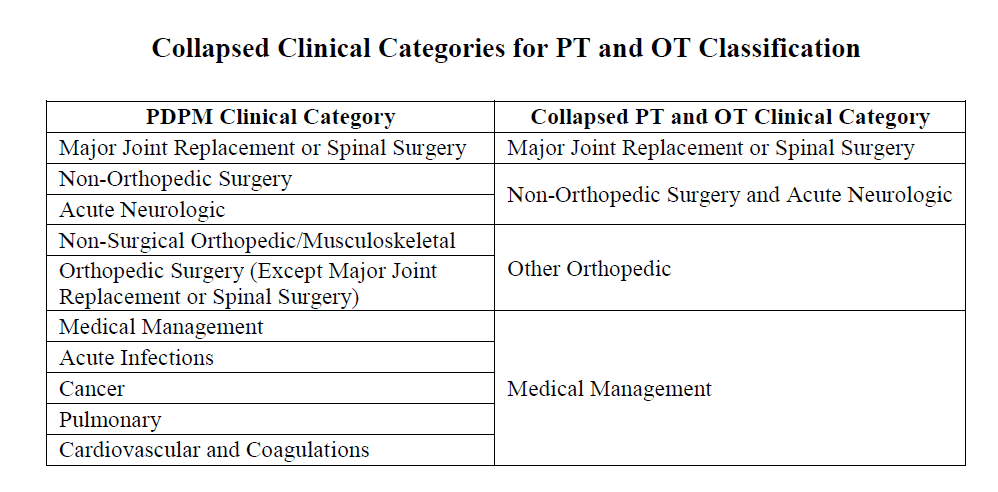
ICD-10 Codes used in MDS Section I0020B as the primary reason for SNF Part A covered care are used for case mix classification under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, or identified as a Return to Provider code [meaning this code cannot be used in Section I0020B of the MDS].
Each year, CMS makes modifications to the mapping of certain ICD-10 Codes related to PDPM. This year, multiple changes are recommended to align PDPM mapping with ICD-10 coding rules.
The proposed code changes for FY 2024 are as follows:
Proposed General ICD-10 Mapping changes:
- From Return to Provider to Medical Management
- D75.84 Other platelet-activating anti-platelet factor 4 (PF4) disorders
- K76.82 Hepatic encephalopathy
- From Acute Neuro to Medical Management
- G90.A Postural orthostatic tachycardia syndrome (POTS)
- From Medical Management to Return to Provider
- F43.81 Prolonged grief disorder and F43.89 Other reactions to severe stress
168 Unspecified Substance Use Disorder Codes from Medical Management to Return to Provider
- Including: F10.90 Alcohol use, unspecified, uncomplicated, F10.91 Alcohol use, unspecified, in remission, F11.91 Opioid use, unspecified, in remission, F12.91 Cannabis use, unspecified, in remission, F13.91 Sedative, hypnotic or anxiolytic use, unspecified, in remission, and F14.91 Cocaine use, unspecified, in remission
- LINK to full list of 168 Substance Use Disorder Codes for Return to Provider
91 Fracture Codes (Displaced and Pathological) – Now Adding Eligibility for One of Two Ortho Surgery Categories
- 45 subcategory S42.2 – codes for displaced fractures
- 46 subcategory of M84.5 – codes for pathological fractures
- LINK to 91 Proposed Clinical Category Changes for S42.2 and M84.5 Fracture Code list
95 Codes added to Return to Provider List as Unacceptable Principal Diagnosis Codes
- Will no longer be able to be used as the primary diagnosis on the claim due to conflict with the Medicare Code Editor system
- LINK to full list of 95 codes now Return to Provider
Here is the link to the new DRAFT ICD-10 Mapping File in the Rule: FY 2024 DRAFT PDPM ICD-10 Mapping (ZIP)
Changes In Wage Index – Geographical Locations – For Medicare Part A Calculation
Providers are deemed “urban” or “rural” for purposes of calculating the labor portion of the daily rate, a factor in determining the overall daily rate for a facility. Using wage index values specific to location to adjust the labor portion of the rate is done to reflect the wage differences throughout the country.
Clearly stated, reimbursement rates are different depending on where you live.
The proposed Wage Index Tables for FY 2024 can be found here:
Not sure if your SNF is classified as urban or rural? Use the Wage Index Look Up Tool HERE
Insert deep breath here….
Changes to CMS Medicare Part A Quality Measure Programs
If you are not already heavily involved in your SNF Quality Measure Program processes, NOW is the time. As these Measure Programs grow and grow, don’t get left behind. By understanding the Measures and Programs, SNF therapy and MDS professionals can be a godsend to their facility. Here, we break down each program and what will be changing.
SNF Quality Reporting Program (SNF QRP)
The SNF QRP is the program that started small over 7 years ago [remember when Section GG was new?] and is now ballooning into the program with the most measures. This is a pay for reporting program, meaning, SNFs are required to report measure data, and if not reported, facilities will continue to be subject to a 2% Part A payment penalty [don’t report…..lose 2% of Part A $$ ]. The penalty occurs when information is missing, not for poor outcomes. [yet]
What does missing data look like? Data can be MDS questions that have missing (dashed) data in select items, or data that is required to be provided directly from the SNF to the CDC’s National Healthcare Safety Network (NHSN).
Here is a link to all the MDS questions that, if not filled out, will trigger the payment penalty if the threshold is met. For the FY2023 collection period, both the current MDS and the “new” MDS are in play, and as of 10/1/23, the list of MDS questions has increased significantly (Thanks to SPADES!).
LINK HERE Make sure MDS staff have this info. These are the MDS items being collected NOW that will potentially impact FY 2025 Annual Payment Update (APU) Determination. The last column includes all the ADDITIONAL MDS QUESTIONS involved starting 10/1/23. Don’t lose 2%!!
Before we jump into what is “proposed,” let’s look at what we currently have to deal with.
Here are the 16 Measures in place for FY2024:
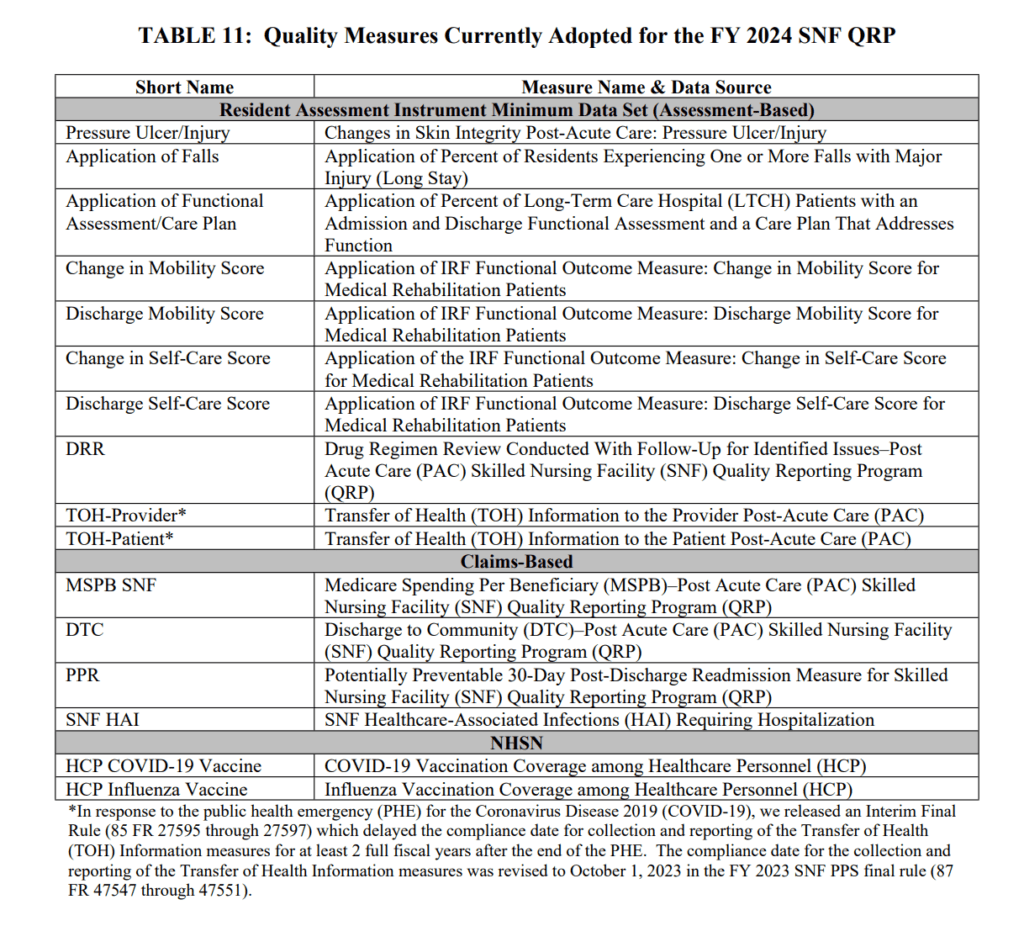
The following measures were discussed in detail HERE, with a quick recap below for the newest 5 of the bunch.
- Transfer of Health Information (Provider and Patient) Measures
- These 2 MDS measures above were on hold during the PHE and were also awaiting changes to the MDS. Now that we have the “new” MDS version starting 10/1/23, this measure is in full swing. Items are on the PPS DC MDS and are tied to reconciled medication lists
- Data collection starts 10/1/23
- SNF Healthcare-Associated Infections Requiring Hospitalization measure (SNF HAI):
- This outcome measure collects data for infections acquired in the SNF resulting in re-hospitalization and is publicly reported
- COVID-19 Vaccination Coverage among Healthcare Personnel (HCP):
- This process measure tracks COVID-19 vaccination coverage among HCP in the SNF setting and publishes rates on Care Compare for the public
- 2% Part A rate penalty for not reporting to CDC’s NHSN
- Influenza Vaccination Coverage Among Healthcare Personnel
- Data collection began 10/1/22 and will be collected annually
- Separate calculations for employees, non-employed licensed independent practitioners (ie: MD), students and volunteers, and contract staff.
- 2% Part A rate penalty for not reporting to CDC’s NHSN
- Standardized Patient Assessment Data Elements (SPADES)
- CMS adopted SPADES for the following categories collected on the MDS:
- Cognitive function and mental status
- Special services, treatments, and interventions (e.g., need for ventilator, dialysis, chemotherapy, and total parenteral nutrition)
- Medical conditions and comorbidities (e.g., diabetes, heart failure, and pressure ulcers)
- Impairments (e.g., incontinence; impaired ability to hear, see, or swallow)
- Data collection will start 10/1/23 on selected SPADES with new MDS Item Set Questions
- 2% Part A rate penalty for not reporting
- Link to Measure information
- CMS adopted SPADES for the following categories collected on the MDS:
Greater Chance for 2% Payment Penalty
As the list of measures continues to grow, there is a greater chance of missing information and incurring a 2% payment penalty. Not only do 80% of MDS assessments need to contain 100% of the SNF QRP required data from the MDS, SNFs also need to submit 100% of data for the COVID-19 and Influenza Vaccination for Healthcare Personnel to the CDC NHSN system. If info is missing either way, the penalty will apply. This does not leave much room for error.
To make this even more challenging…
In the Proposed Rule, CMS would like to increase the required MDS data threshold from 80% to 90% beginning with data collected 1/1/2024, for a payment impact on 10/1/25.
Now On to the Newly Proposed Items….
While we are still digesting the new MDS that will go into effect 10/1/23, the Proposed Rule outlined SNF QRP changes for 2025 and 2026. Though these dates may seem far away, keep in mind that the SNF QRP works in 2 time tables, collecting data NOW for payment impact in the FUTURE. So though we may want to push this information to next year’s to-do list, it needs to be absorbed NOW.
3 New Measures:
- Discharge Function Score Measure (FY2025)
- Outcome measure from Section GG Self Care and Mobility Technical Report
- Calculated % of Part A residents who meet or exceed DC Function Score
- Uses 10 GG items: Eating, Oral Hygiene, Toileting Hygiene, Roll L/R, Lying to Sit, Sit to Stand, Transfer, Toilet Transfer, Walking 10′ and Walking/Wheeling 50′
- This will replace the original GG Measure “Application of Functional Assessment / Care Plan, ” a.k.a Do you have at least 1 Section GG DC Goal set?
- Reporting starts 10/1/2023
- COVID-19 Vaccine: Percent of Patients/Residents “Who Are Up to Date” Measure (FY2026)
- Adding MDS items to track if residents are “up to date”
- Reporting starts 10/1/2024
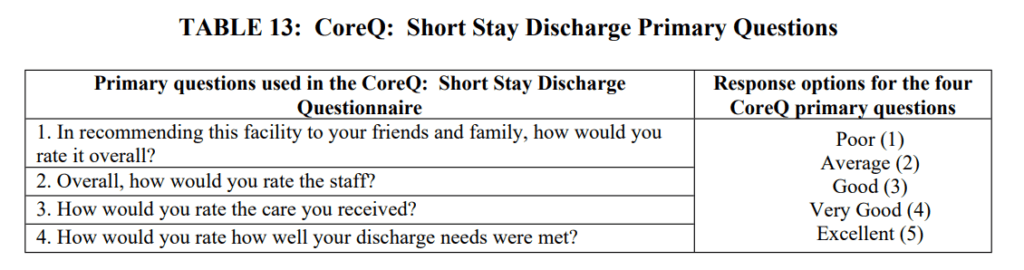
- CoreQ: Short Stay Discharge Measure (FY2026)
- Targets Part A short term residents of less than 100 days
- Measures the % of residents discharged in a 6 month period who are satisfied with stay
- See the 4 questions below:
1 Measure Modification
- COVID-19 Vaccination Coverage among Healthcare Personnel Measure (FY2025)
- Report the number of HCP who are up to date with recommended COVID-19 vaccinations
- Used to say “completed 1st vaccination course,” and will now include boosters
- Data reporting starts 10/1/23, Public reporting 10/1/24
3 Measure Removals (involving Section GG effective FY2025)
- Admission and Discharge Functional Assessment /Care Plan That Addresses Function (1 DC Goal)
- Change in Self-Care Score
- Change in Mobility Score
On to the LAST QM Program….
SNF Value-Based Purchasing Program (SNF VBP)
Since it’s inception, this Program has only had 1 measure….until now…
What is this Program?
The SNF VPB works by reducing Medicare Part A payments to ALL SNFs by 2% and then allows for an opportunity to recoup part of the 2% by demonstrating success with the established Measure.
Since the start of this Program, there has only been 1 Measure: The SNF 30-Day-All-Cause Readmission Measure, which measures if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital.
With Measures included in the Proposed Rule, this is the full list of adopted and proposed Measures:
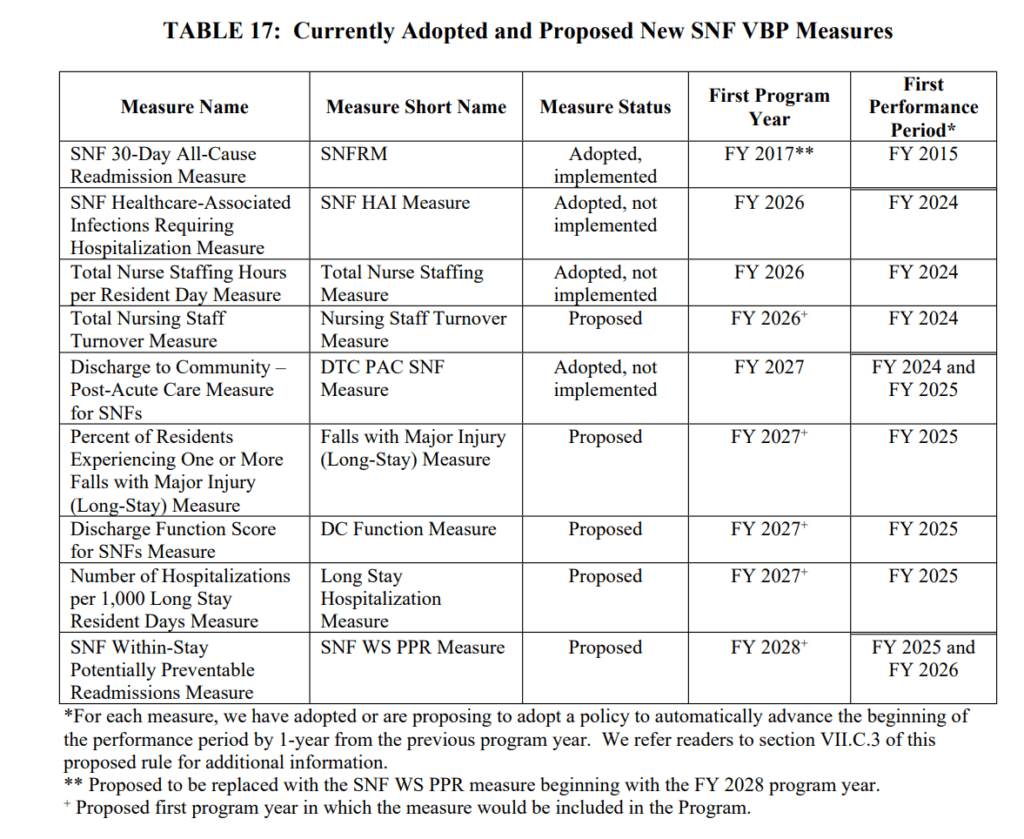
Performance Periods for these 4 Measures start 10/1/23
- SNF HAI Requiring Hospitalization (Adopted last year)
- Total Nurse Staffing Hours per Resident Day (Adopted last year)
- Total Nursing Staff Turnover (Effective 10/1/25)
- Proposed this year, to be added to the Total Nurse Staffing Hours above
- Using PBJ data; Impacts 5 Star Rating
- DC to Community (Adopted last year)
and don’t forget the original Measure of this Program, for a total of 5 Measures 10/1/23.
MDS-Based Measures (Data collection 10/1/24, Affects payment 10/1/26)
- Falls with Major Injury (Includes long stay residents)
- Already a QM in other programs, used in 5 Star and publicly reported
- Data collection starts 10/1/24
- Discharge Function Score
- Same Measure from SNF QRP
- Uses Section GG
- Data collection starts 10/1/24, impacts payment 10/1/26
Claims-Based Measures
- # of Hospitalizations per 1,000 long stay resident days
- Already publicly reported and used for 5 Star
- Data collection starts 10/1/24
- SNF With-Stay Potentially Preventable Readmission Measure (FY2028)
- Replace the SNFRM with a modification of the previously proposed “SNF Potentially Preventable Readmission After Hospital DC Measure.”
- Data collection FY2025 and 2026 for payment impact FY2028
The SNF VBP rule also proposes to increase the amount SNFs are eligible to receive back for “good performance,” and also proposes a “Health Equity Adjustment,” or a bonus, for top performing SNFs that have 20% of dual eligible (Medicare + Medicaid) residents in the period.
What’s Next?
CMS is accepting comments for the proposed rule through June 5, 2023. We know from past results that comments submitted have the potential to influence CMS decisions. Consider commenting on an area you are passionate about. You never know! Electronic comments can be made at https://www.regulations.gov Follow the “Submit a comment” instructions.
Additional Resources:
HERE is a link to the Proposed Rule. PDF Version
HERE is a link to the CMS Fact Sheet.
PDPM Calculators and Resources HERE
If you have any questions, send them to our Just Ask Q&A Forum and we will reach out to you to get your questions answered.
Thank you for all you are doing to provide the best care to the geriatric population!
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
President | Montero Therapy & MDS Resource Team
MonteroTherapyServices.com

The CMS Quality Measures impact outcomes & reimbursement for your SNF.
Mastering the components of each Measure Program is a must for SNF therapy professionals.
Be a leader in this specialized area of practice!