If all goes as proposed by CMS in the recent release of the Medicare Part A Skilled Nursing Facility Prospective Payment System (SNF PPS) FY2021 Proposed Rule, SNF therapy professionals will have a chance to catch their breath!
The proposed changes for 10/1/20 are minimal in comparison to years past, resulting in a document to digest that is less than half the typical size. The 36 page Proposed Rule [CMS-1737-P] can be downloaded from the Federal Register HERE.
Let’s take a quick look at the highlights that are most pertinent to SNF therapy professionals.
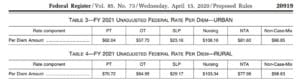
Medicare Part A Payment Rate Changes
The Federal Per Diem rates are updated annually. On 10/1/20 the rates for Part A will increase by 2.3% which equates to approximately $784 million more for SNFs. These are the unadjusted rates that when multiplied by the case mix index values then determine each PDPM Case Mix Group rate.
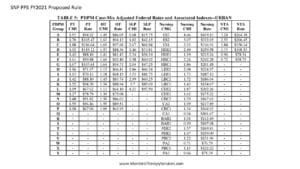
Medicare Part A PDPM Changes – Case Mix Index Values
Case Mix Index values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, will not change for FY2021. When multiplied by the Unadjusted Federal Per Diem Rate shown above, Case Mix Group rates will look something like this for 2021 (Urban).
Medicare Part A PDPM Changes – ICD-10 Code Mapping for PT and OT Component
ICD-10 Codes used in MDS Section I0020B as the primary reason for SNF Part A covered care are used for case mix classification under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, or identified as a Return to Provider code [meaning this code cannot be used in Section I0020B of the MDS]. In the Proposed Rule, CMS has made some adjustments to the mapping, as well as added and deleted additional codes.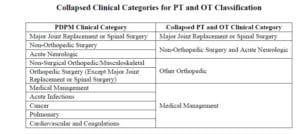
First, as a result of the National Emergency, ICD-10 Code U07.1 “COVID-19” was added to the current list of codes (this code is in effect now) and maps to Pulmonary and Medical Management. To view the CMS ICD-10 Mapping Tool updated 3/31/20 with the new code, CLICK HERE. By 10/1/20, a new mapping tool will be released for use to include the additional code changes, as follows:
- Remapping certain Cancer ICD-10 Codes to allow for combination with specific Section J surgical procedures to increase the category from Medical Management to a “Non-Orthopedic Surgical” category. (Codes range from C15 to C80.1 and D37.09 to D49.7)
- Adjusting the default Clinical Category for Lumbar Vertebral Fracture from “Ortho Surgery” or “Major Joint Replacement” to “Non-Surgical Ortho” when no surgery has occurred (ie: S32.031D, S32.19XD, S82.001D and S82.002). These codes may then be eligible for “One of the Two Ortho Surgery” categories depending on how Section J is answered.
- Remapping a handful of ICD-10 Codes for Spinal Stenosis (M48-M48.08) to be eligible for “One of the Two Orthopedic Surgical” categories if specific items in Section J are checked.
- Remapping a handful of ICD-10 Codes for Surgical Aftercare to be eligible for “Non-Orthopedic Surgical” categories if specific items in Section J are checked. (Z48.0 series of codes)
- Assigning “Return to Provider” for some of the less specific fracture codes (ie: S82.009A, S82.013A, S82.016A, S82.023A, S82.026A, S82.033A, S82.036A and S82.099A)
Medicare Part A PDPM Changes – ICD-10 Code Mapping for the Non-Therapy Ancillary Component
Non-Therapy Ancillary Component points are derived from either checking specific diagnoses on the MDS, or adding the ICD-10 Code to Section I8000. Codes for use in I8000 with corresponding point value are provided by CMS in the NTA Mapping Tool. In the Proposed Rule, there is 1 noted change in the list of ICD-10 codes used to identify “Complications of Specified Implanted Device or Graft.” The ICD-10 codes that can be included in I8000 of the MDS to capture 1 NTA point for this category will be reflected in the new mapping tool.
Changes to the Minimum Data Set (MDS)
In December of 2019, CMS posted a draft of the MDS 3.0 item set to be implemented 10/1/20. Major changes were proposed, including the removal of Section G from OBRA assessments. On March 19th, 2020, CMS announced that the MDS changes planned for October 1, 2020 would be delayed. Read HERE for more information.
Changes In Wage Index – Geographical Locations – For Medicare Part A Calculation
Providers are deemed “urban” or “rural” for purposes of calculating the labor portion of the daily rate, a factor in determining the overall daily rate for a facility. Using wage index values specific to location to adjust the labor portion of the rate is done to reflect the wage differences throughout the country. [Reimbursement rates are different depending on where you live.] The Rule is proposing that a small number of counties previously listed as urban will switch to rural and vice versa. Use the list below to see if your county was impacted.
Not sure if you are urban or rural? Use the Wage Index Table below to look up your county.
Changes to CMS Medicare Part A Quality Programs
- SNF Quality Reporting Program (SNF QRP)
- The SNF QRP is the program behind Section GG, as well as other MDS data collection to measure multiple areas of care. Think skin….falls….function. There are no proposed changes to the SNF QRP for FY2021! Data collection for the multiple measures in this program will continue, and facilities will continue to be subject to a 2% Part A payment penalty for submission of Part A MDS’s with missing (dashed) data in select items.
- SNF Value-Based Purchasing Program (SNF VBP)
- The SNF VBP Program is the one that reduces Medicare Part A payments to all SNFs by 2% and then allows for an opportunity to recoup all or part of the 2% by demonstrating success with the established Quality Measure, SNF 30-Day-All-Cause Readmission Measure. In essence, this measures if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital. The Rule included the Achievement Threshold and Benchmark data for FY2023 as pictured here, though no significant changes were made to the program for FY2021 that will impact SNF therapy.
Additional Changes In The Coming Months
SNFs have multiple regulatory changes coming at them almost daily due to the National Emergency and COVID-19. Waivers for Part A technical requirements including 3 midnight stay and 60 day spell of wellness are currently in place, though will likely expire prior to the Final Rule. These articles will help explain all the recent changes.
COVID-19 Part A and Part B Changes
CMS Issues Critical Recommendations to SNFs
SNF professionals have a lot to keep track of these days! Visit our SNF COVID-19 Resource Page to help stay on top of the changes.
If you have any questions, send them to our Just Ask Q&A Forum and we will reach out to you to get your questions answered.
In your corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Rehab & MDS Compliance Professionals | www.MonteroTherapyServices.com