PDPM and Part A Updates
CMS released the Medicare Part A Skilled Nursing Facility Prospective Payment System (SNF PPS) FY2022 FINAL RULE last week. The Rule contains the components that will go into effect 10/1/21.
The Final Rule contains all the “usual,” with updates to Part A rates, ICD-10 code mapping for PDPM, SNF Quality Reporting Program (SNF QRP) changes, and SNF Value Based Purchasing (SNF VBP) updates.
The Rule also addresses the biggest concern from the Proposed Rule.… The PDPM Parity Adjustment, otherwise defined as “how SNFs will pay back the $1.7 Billion overpayment for the first year of PDPM.”
Let’s take a look at the key points SNF therapy professionals need to be aware of.
Medicare Part A Payment Rate Changes
The Federal Per Diem rates are updated annually and kick in every October 1st. This “raise” SNFs receive is typically over 2%. However, this October, SNFs will see a 1.2% rate increase, which equates to approximately $410 million more in payments as compared to 2021. That may sound like big bucks but remember, there are over 15,000 SNFs that share this pot!
This 1.2% increase for FY2022 was set to be a market basket increase of 2.7% before corrections were made, reducing the rate by 1.5% {Forecast error correction of 0.8%, 0.7% multi-factor productivity adjustment}. In addition to those corrections, a reduction of an additional $1.2 million was built in to account for changes made with shifting dollars from Part A to Part B for Blood Clotting Factor exclusions explained in the Consolidated Billing section below.
Here are the new unadjusted rates for October 1st. Think of “unadjusted” a few ways:
- These rates are not yet adjusted for where your SNF lives….city, state, urban or rural classification
- The rates still have to be multiplied by the case mix index value to determine each PDPM Case Mix Group daily rate
- These rates are prior to any PDPM variable per diem rate adjustments for PT/OT and NTA components
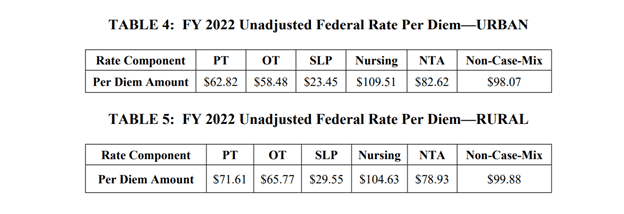
To give you an idea of the daily rate changes [urban] from FY2021 to FY2022, the PT Component will increase $0.78/day, OT $0.73/day, SLP $0.29/day, Nursing $1.35/day, NTA $1.02/day and the Flat Rate $1.22/day. [Don’t hold your breath for that raise!]
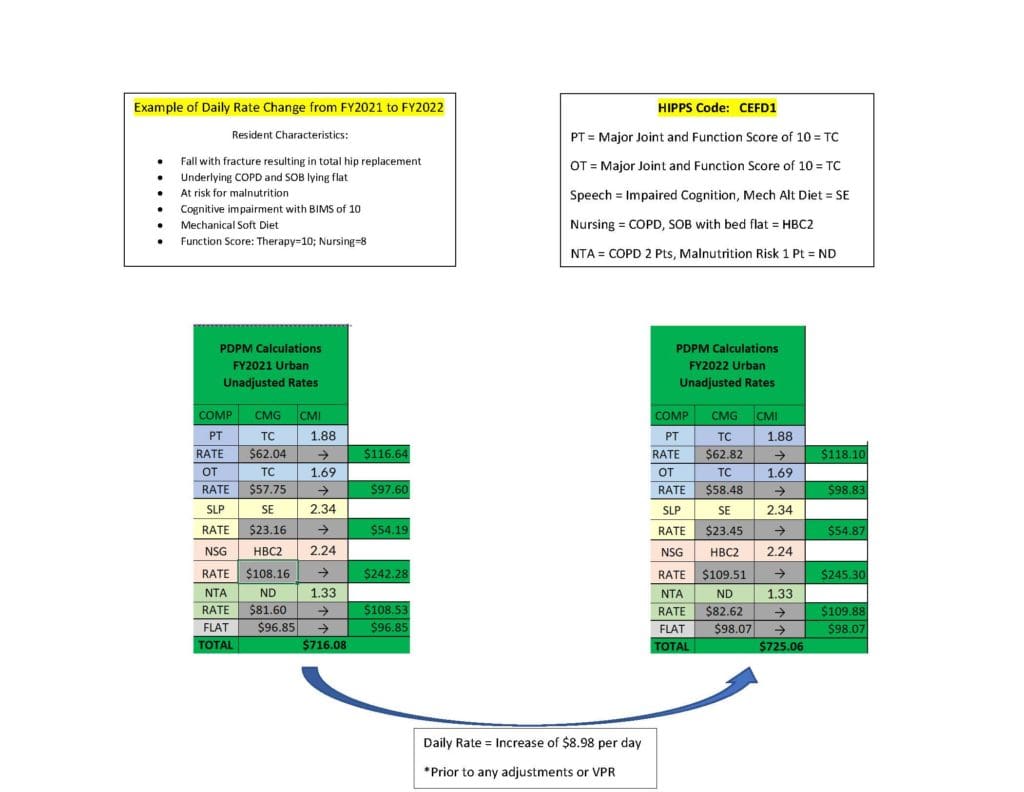
Rate Change Impact on Sample Total Joint Resident
Below is a comparison of the FY2021 and FY2022 daily rate for a resident with the characteristics described below. With the same HIPPS code, the overall increase in payment is approximately $9 per day. The PDPM Calculator below can be used to determine rates for any HIPPS code.
PDPM Rate Recalibration – 1 Year Pass!
The Proposed Rule included a section that caused some concern called, “Recalibrating the PDPM Parity Adjustment.” In this section, CMS shared therapy data and provider practice patterns that knocked PDPM off its’ budget neutral pedestal, by $1.7 Billion (or 5%), and discussed the necessary “recalibration” {payback} that will be required.
This recalibration will happen and will impact all the above rates….but not this year. We will find out how this will play out when the Proposed Rule is released next Spring.
The Proposed Rule figures included the potential for PT and OT rates decrease an average of $5 per day each, Speech averages a $3 decrease per day, and Nursing and NTA a $5-26 and $3-15 per day decrease per CMG respectively {and remember, each component is added together to make the total daily rate} {Yikes!} If you compare the recalibrated rates with today’s rates, the recalibrated rates are significantly lower. Depending on the component combinations, the rate could be $10-48/day lower. That’s significant! {So forget that raise for the next few years as well!}
To learn more about the therapy data CMS shared, as well as the PDPM recalibration options from the Proposed Rule, CLICK HERE to read more.
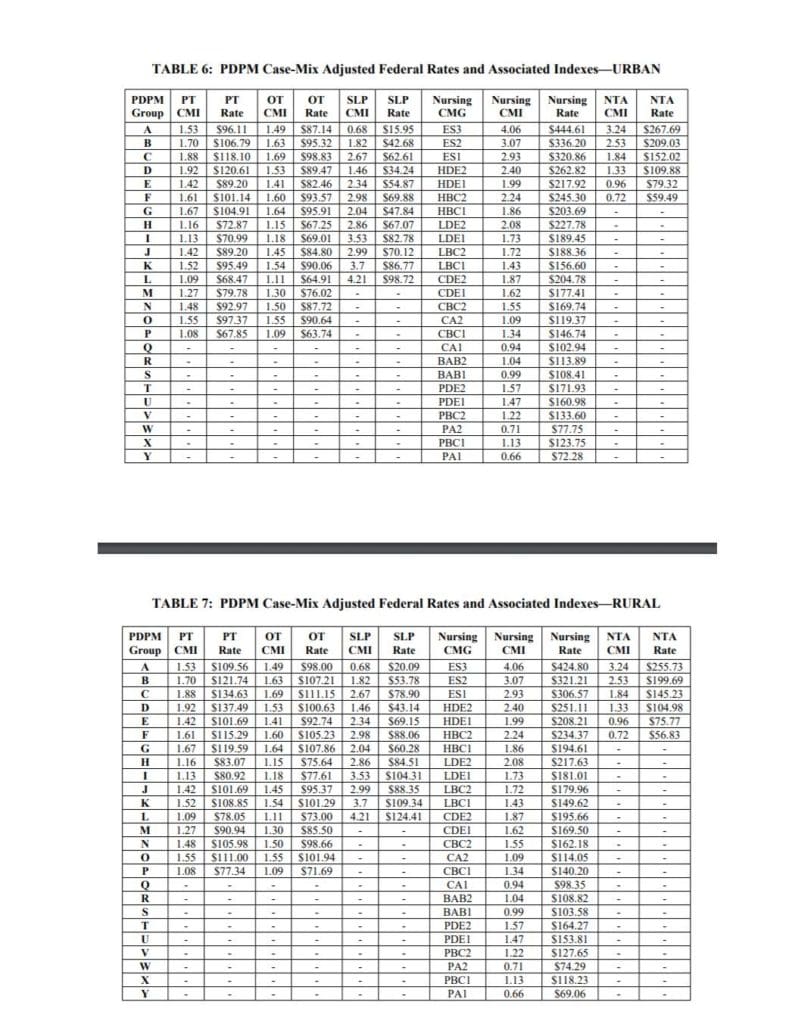
PDPM Case Mix Index Values
Case Mix Index (CMI) values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, are not changing for FY2022 {more on that below…} When multiplied by the Unadjusted Federal Per Diem Rate shown above, Case Mix Group rates will look something like this for FY2022 (Urban and Rural). The resulting dollar differences for the DAILY RATE are due to the updates in the Federal Unadjusted Rates above.
PDPM Changes – ICD-10 Code Mapping for PT, OT and Speech Components
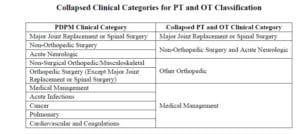
ICD-10 Codes used in MDS Section I0020B as the primary reason for SNF Part A covered care are used for case mix classification under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, or identified as a Return to Provider code [meaning this code cannot be used in Section I0020B of the MDS].
All the ICD-10 Codes Identified in the Proposed Rule will be adopted:
- D57.42 “Sickle-cell thalassemia beta zero without crisis” and D57.44 “Sickle-cell thalassemia beta plus without crisis” currently mapping to Medical Management will map to Return to Provider
- K20.81 “Other esophagitis with bleeding”, K20.91, “Esophagitis, unspecified with bleeding, and K21.01 “Gastro-esophageal reflux disease with esophagitis, with bleeding” currently mapping to Return to Provider will map to Medical Management.
- M35.81 “Multisystem inflammatory syndrome”, currently mapping to Non-Surgical Orthopedic/Musculoskeletal will map to Medical Management
- P91.821 “Neonatal cerebral infarction, right side of brain,” P91.822, “Neonatal cerebral infarction, left side of brain,” and P91.823, “Neonatal cerebral infarction, bilateral,” currently mapping to Return to Provider will map to Acute Neurologic
- U07.0, “Vaping-related disorder,” currently mapping to Return to Provider will map to Pulmonary / Medical Management
- G93.1 “Anoxic brain damage, not elsewhere classified” will change from Return to Provider to Acute Neurologic
We also received a new FY2022 Mapping Tool for all the ICD-10 Codes that can be downloaded below:
Changes In Wage Index – Geographical Locations – For Medicare Part A Calculation
Providers are deemed “urban” or “rural” for purposes of calculating the labor portion of the daily rate, a factor in determining the overall daily rate for a facility. Using wage index values specific to location to adjust the labor portion of the rate is done to reflect the wage differences throughout the country. [Reimbursement rates are different depending on where you live.] There was a significant update in this area effective 10/1/20. The updated Wage Index Tables for FY 2022 can be found below.
Not sure if you are urban or rural?
Visit the CMS Wage Index Home Page for more information, or Download the FY2022 Final Rule Wage Index Tables below.
Changes to Consolidated Billing
The Final Rule established an additional category of excluded codes from consolidated billing requirements, specific to certain blood clotting factors and services for the treatment of hemophilia and other bleeding disorders. The specific items and services are those identified by codes J7170, J7175, J7177–J7183, J7185–J7190, J7192–J7195, J7198–J7203, J7205, and J7207–J7211. Based on input received after the Proposed Rule, the Final Rule also added codes J7204, J7212 for blood disorders, and Q5123 for the chemotherapy drug, Riabni.
These exclusions impact the Part A rates as previously mentioned by shifting the $1.2 million from Part A to Part B, and as such, adjustments to the Part A rates from the NTA and Nursing Components of PDPM are included.
The latest list of excluded codes can be found on the SNF Consolidated Billing website at https://www.cms.gov/Medicare/Billing/SNFConsolidatedBilling.
Changes to CMS Medicare Part A Quality Programs
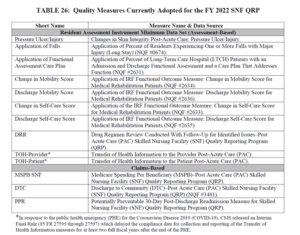
SNF Quality Reporting Program (SNF QRP)
- The SNF QRP is the program behind Section GG, as well as other MDS data collection to measure multiple areas of care. Think skin….falls….function. This is a “pay for reporting program,” and data collection for the multiple measures will continue. Facilities will continue to be subject to a 2% Part A payment penalty for “not reporting,” by submission of Part A MDS’s with missing data in select items…. AKA “dashes.”
- 2 Key points to remember with the SNF QRP Measures:
- The 2% penalty comes from not reporting the data, not the data content
- The data is typically being collected long before it has to be reported
- Here are the 13 Measures in place for FY2022:
- CMS will adopt two new measures for the SNF QRP beginning with FY 2023:
- SNF Healthcare-Associated Infections Requiring Hospitalization measure (SNF HAI)
- This is an outcome measure using claims data, and per CMS, “the data would allow providers to exchange and compare outcomes across the care continuum and Post Acute Care (PAC) settings.” “Clinical data captured in every clinical setting informs a resident’s current care plan, facilitates coordinated care, and improves Medicare beneficiary outcomes,” and CMS plans to develop HAI measures in other PAC settings, such as the Inpatient Rehabilitation Facility (IRF) Quality Reporting Program and the Long-Term Care Hospital (LTCH) Quality Reporting Program. This measure would estimate the risk-standardized rate of HAIs that are acquired during SNF care that result in hospitalization, using 1 year of Medicare FFS claims. The measure would include multiple infection types (sepsis, UTI, pneumonia) and compare SNFs to their peers.
- CMS will begin by using FY2019 claims, and the outcomes will be publicly reported next year
- COVID-19 Vaccination Coverage among Healthcare Personnel (HCP)
- CMS identified this process measure as a priority in response to the current public health crisis. This process measure was developed with the Centers for Disease Control and Prevention (CDC) to track COVID-19 vaccination coverage among healthcare staff in the SNF setting.
- CMS states the importance of requiring SNFs to report staff vaccinations in order to assess whether they are taking steps to limit the spread of COVID-19 among their workers, reduce the risk of transmission of COVID-19 within their facilities, and to help sustain the ability of SNFs to continue serving their communities throughout the PHE and beyond.
- Under the May 8, 2020 Interim final rule, SNFs are required to submit COVID-19 data through the CDC’s NHSN Long-term Care Facility COVID-19 Module of the NHSN. Examples of data reported in the module include: suspected and confirmed COVID-19 infections among residents and staff, including residents previously treated for COVID-19; total deaths and COVID-19 deaths among residents and staff; personal protective equipment and hand hygiene supplies in the facility; ventilator capacity and supplies available in the facility; resident beds and census; access to COVID-19 testing while the resident is in the facility; and staffing shortages. Although HCP and resident COVID-19 vaccination data reporting modules are currently available through the NHSN, the reporting of this data is voluntary.
- CMS states they believe that publishing facility-level COVID-19 HCP vaccination rates on Care Compare would be helpful to many patients, including those who are at high-risk for developing serious complications from COVID-19, as they choose facilities from which to seek treatment.
- CMS will use {minimal} data from 1 week in Oct, Nov and Dec 2021. to represent the reporting next year….a potential additional factor in the crunch to get vaccinated.
- Transfer of Health (TOH) Information
- CMS updated the denominator for this quality measure to remove patients discharged home with home health or hospice. This measure is currently not in place and will begin in FY2023.
- SNF Healthcare-Associated Infections Requiring Hospitalization measure (SNF HAI)
SNF Value-Based Purchasing Program (SNF VBP)
- The SNF VBP Program is the one that reduces Medicare Part A payments to all SNFs by 2% and then allows for an opportunity to recoup all or part of the 2% by demonstrating success with the established Quality Measure, SNF 30-Day-All-Cause Readmission Measure. In essence, this measures if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital.
- As Proposed, CMS is adopting a policy for FY2022 that will suppress the use of SNF readmission measure data for purposes of scoring and payment adjustments in the SNF VBP Program. CMS states this “is a necessity to ensure that the SNF VBP program does not reward or penalize facilities based on factors that the SNF readmission measure was not designed to accommodate.”
- All SNFs participating in the FY 2022 SNF VBP program will be assigned a performance score of zero, resulting in identical performance scores and identical incentive payment multipliers. The 2% reduction will apply, followed by a 60% return of the 2% (a 1.2% payback). The other 40% stays with Medicare. There is an exception for SNFs with less than 25 eligible stays, allowing these SNFs the full 100% payback.
- CMS will use the following 12 months for reporting FY2022: 4/1/19 to 12/31/19, and 7/1/20 to 9/30/20.
- CMS also outlines consideration for additional VBP measures for future years, including: functional status, patient safety, and care coordination, as well as including measures expanded to all residents, not only Part A, and is requesting public comment. See this article for the measures and details presented in the Proposed Rule that remained in the Final Rule.
In Summary
We have 2 full months to digest the new material! Waivers for the PHE are still in place and we are expected to receive 60-days advanced notice of the end date. You can read more about that HERE.
HERE is a link to the Final Rule. [PDF Copy HERE]
HERE is a link to the CMS Fact Sheet.
If you have any questions, send them to our Just Ask Q&A Forum and we will reach out to you to get your questions answered.
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team